Post-operative Extensively Drug Resistant Mycobacterium Tuberculous Discitis
Volume 1 | Issue 1 | Apr – June 2016 | Page 47-49|Dhiraj Vithal Sonawane[1], Eknath Pawar[2], Ajay S Chandanwale[3],Ambarish A Mathesul[3], Abhishek Salunke[4], Swapnil M Keny[1].
Authors :Dhiraj Vithal Sonawane[1], Eknath Pawar[2], Ajay S Chandanwale[3],Ambarish A Mathesul[3], Abhishek Salunke[4], Swapnil M Keny[1]
[1] Department of Orthopaedics, Grant Medical college, & Gokuldas Tejpal Hospital, Mumbai
[2] Department Of Orthopaedics, Grant medical college, Mumbai.
[3] Sasoon Hospital & BJMC, Pune
[4] Gujarat Cancer Research Institute
Address of Correspondence
Dr. Dhiraj V. Sonawane
Grant Medical college, & Gokuldas
Tejpal Hospital, Mumbai
Email: dvsortho@gmail.com
Abstract
Mycobacterium tuberculosis (MTB) as a cause of postoperative discitis is extremely rare. We report a first case of extensively drug resistant mycobacterium tuberculosis (XDR-TB) as cause of early postoperative discitis, confirmed on culture and sensitivity. XDR-TB is looming threat and remains a challenge in management .Even with present day available treatment options the prognosis remains poor. Reviewing the literature we discuss possible management in XDR TB discitis.
Introduction
Post-operative discitis is an uncommon but devastating complication after invasive spinal procedure [1, 2]. The incidence of post procedural discitis ranges from 0.26 to 4% [2]. Most common organisms responsible are Staph. aureus and streptococcus species. Three cases of postoperative discitis due to mycobacterium tuberculosis are reported in English literature [3, 4, 5]. XDR TB by WHO global task force on XDR TB, is defined as TB which is resistant to isoniazid and rifampin, plus resistant to any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin). XDR-TB & TDR-TB (totally drug resistant tuberculosis) continues to pose challenge to control program and treating physician [6, 7, 8, 11]). We report 1st case of XDR TB discitis and discuss possible therapeutic options.
Case report:
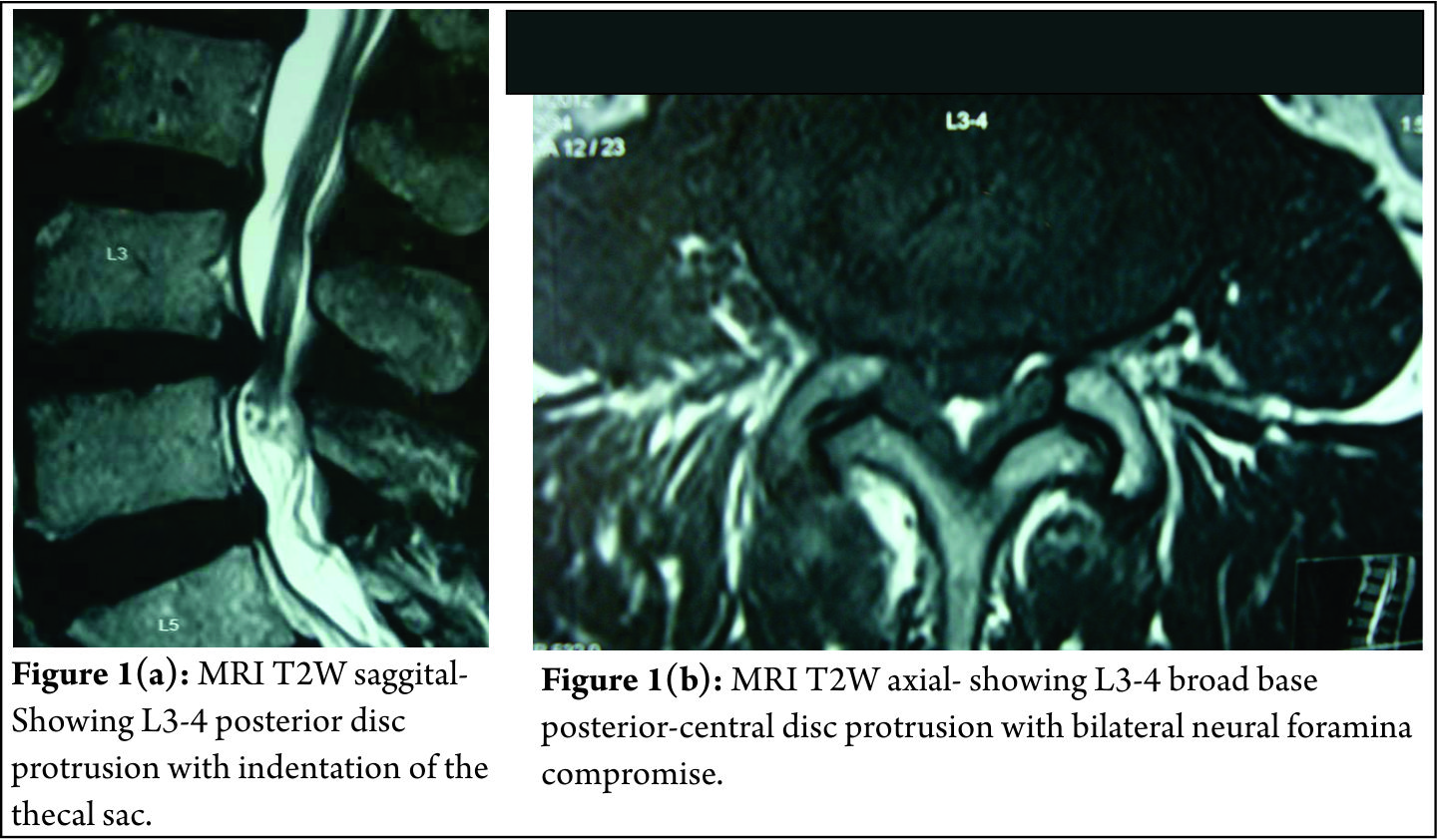
A 61 year old male, known case of diabetes and hypertension was operated with laminectomy and discectomy for L3-4 disc prolapse in December 2010 (Fig 1a, b).
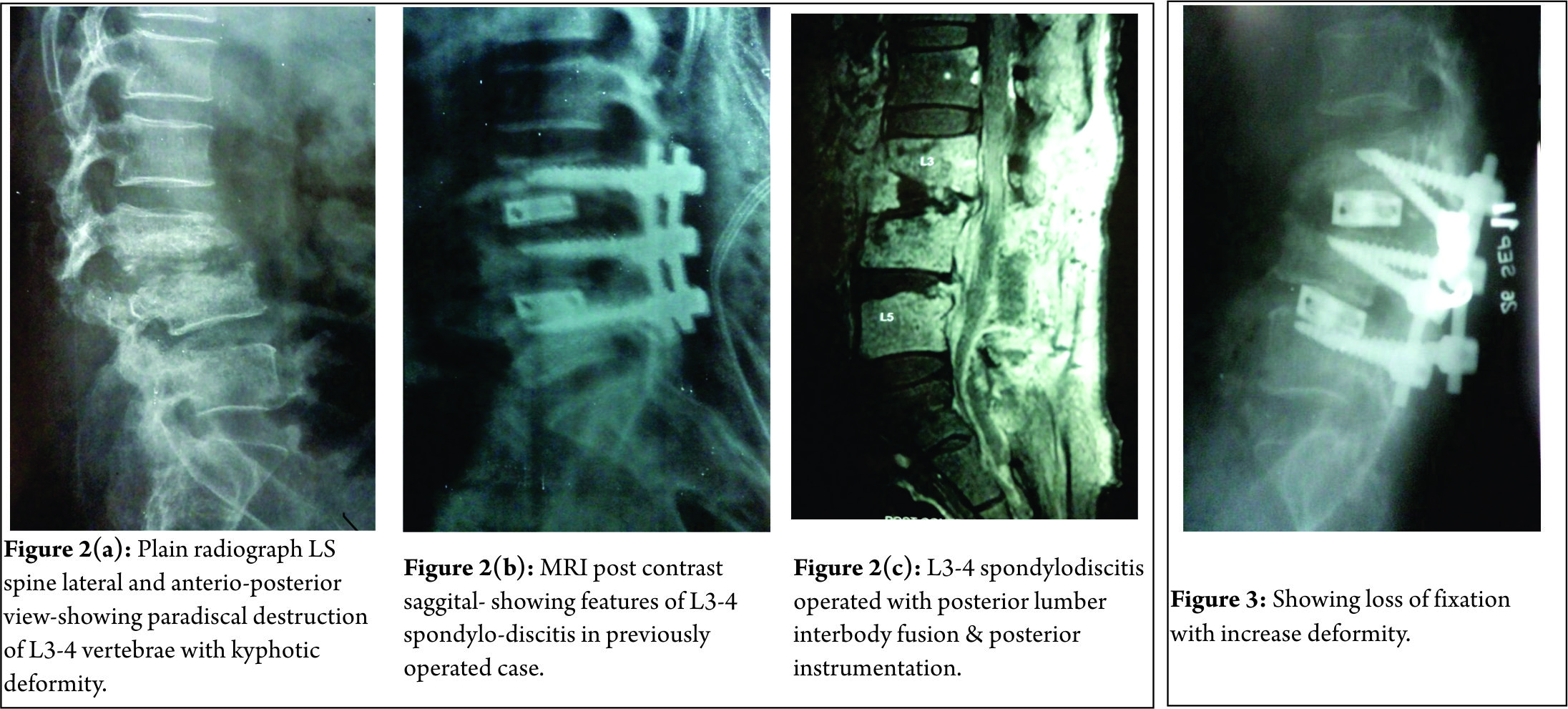
Pre operatively patient had left ankle dorsiflexion MRC grade 3 and depressed left knee reflex. Neurological status remained same after surgery. Three weeks after surgery, patient developed seropurulent discharge through the operated wound. Erythema and induration was present on upper end of wound. Hematological investigation showed TLC- 17,000/ cmm, ESR- 48 mm at end of one hour and CRP 4 mg/dl. Pus culture of discharge grew Pseudomonas aeruginosa. Antibiotics were given according to sensitivity for a period of 4 months, but discharge through the wound continued. Plain radiographs 4 months after surgery showed destruction of L3-4 vertebral end plates with lumbar kyphosis (Fig. 2a). MRI demonstrated altered marrow signal in L3, 4, 5 vertebral bodies with epidural soft tissue causing compression of dural sac, suggesting L3-4 infective spondylodiscitis (Fig 2b). Surgical debridement was done. Intra operative sample from disc space revealed acid fast bacilli on staining. On retrospective evaluation, patient had no past or family history of tuberculosis (TB) or TB contact. X-ray chest was normal. Patient was started on Isoniazid (H) 300mg, Rifampicin (R) 450mg, Ethambutol (E) 600mg & Pyrazinamide (Z) 750mg daily. BACTEC report at 4 weeks showed mycobacterium tuberculosis resistant to all the 1st and most of 2nd line anti tuberculosis drugs (ATT) including ciprofloxacin and kanamycin but sensitive to Amikacin and Clarithromycin. Four drug ATT was discontinued. Patient was started on PZA, Levofloxacin, cycloserine, and Amikacin as per advice of TB physician. After 2 weeks, discharging sinuses with pale granulation at the opening developed. Another surgical debridement with interbody fusion (cage and bone grafting) and posterior stabilization was done (Fig 2c). However, patient’s condition did not improve. ESR (68mm/hour) and CRP (5.8 mg/dl) remained elevated. Because of the rising serum creatinine level (2.5 mg %), Amikacin was discontinued. The follow up radiograph at 1 month post surgery showed vertebral destruction with implant loosening and progression of the kyphotic deformity (Fig. 3). Eighty eighth day postoperatively, patient status deteriorated suddenly and he developed sudden altered sensorium and neck stiffness. He was intubated and kept on vertilatory support, however his condition kept on deteriorating and he died on ninety first postoperative day. The suspected cause of death was meningitis. No Autopsy was performed.
Discussion:
The incidence of post-operative discitis is 0.7 to 0.8 % after antibiotic prophylaxis [1,2]. Discitis results due to haematogenous spread in pediatric age group and by direct inoculation in adults [2]. In TB it possibly spreads from adjacent involved urinary tract [3]. The common organisms are staph. aureus, strep. species, and anaerobic organisms. Other rare organism includes, Mycobacterium tuberculosis (MTB), Candida albicans, Mycobacterium cheloni, Propionibacterium acne [2,3]. The risk factors associated are diabetes, malnutrition, smoking, obesity, alcohol abuse and instrumentation. Early post-operative infection usually presents as wound dehiscence and discharge within 3months of surgery, while late post-operative infection may present within 7 years of surgery with milder symptoms. MRI with contrast enhancement is modality of choice with specificity (93%) and sensitivity (96%) for detection of vertebral infection. [2, 3] In recent years because of use of broad spectrum antibiotics and increased number of people with immunocompromised status there is rise in infections secondary to unusual organisms like MTB [12].On literature search, we found 3 reported cases of post-operative discitis due to M.TB [3,4,5]. Jeon DW et al [4] reported a case of post L4-5 discectomy, MTB spondylodiscitis with bizarre course. MRI showed feature of spondylodiscitis. The biopsy sample was positive for TB PCR specific for MTB. Patient was managed with curettage and interbody fusion using autologous iliac bone grafting and antituberculous therapy (ATT). Patient showed successful fusion and clinical improvement. Iraj lotfinia et al [3] reported similar case of post L4-5 discectomy due to MTB. Patient was managed conservatively with HRZE for 2 months and HR for 10 months, with good outcome. Kaplan ES [5]reported a case of post L4-5 discectomy tuberculous abscess, successfully treated with 3 drugs ATT.
The management for post-operative discitis is conservative approach with organism specific antibiotics and bracing. Those patients who fail to respond to above treatment, with continued pain, infection, spinal deformity require an operative intervention consisting of anterior debridement and interbody fusion with autologous bonegraft and posterior stabilization.
The available treatment options for XDR-TB includes use of later generation fluoroquinolone (levofloxacin, moxifloxacin, sparfloxacin) plus addition of likely active drugs (MTB strain susceptible to drugs tested and drugs to which patients had not been previously exposed) plus linezolid [10]. Surgery will help in taking specimen for diagnosis, reducing bacterial load by debridement, with advantage of fusion. In our case, because of the resistant nature of organism and limited therapeutic options the disease progressed and treatment failed. Meta analytic study using later generation cephalosporins, likely active drugs, linezolid and surgery in pulmonary XDR-TB showed a favourable outcome of 43.7% with death of 20.8% patients [10]. The newer drugs in XDR-TB are less effective, more toxic, and costlier [9, 11]. Therefore further research in development of better anti-tuberculosis drugs (ATT) is required.
References
1. Anthony E. Harris, Chrisanne Hennicke, Karin Byers, William C. Welch. Postoperative discitis due to Propionibacterium acnes: a case report and review of the literature . Surgical Neurology 63 2005; 538–541.
2. Jeff S. Silber, Greg Anderson, Alexander R. Vaccaro, Paul A. Anderson, Paul McCormick. Management of postprocedural discitis. The Spine Journal. 2002; 2:279–287.
3. Iraj Lotfinia , Payman Vahedi . Late-onset post-diskectomy tuberculosis at the same operated lumbar level: case report and review of literature . Eur Spine J 2010;19 (Suppl 2):226–232 .
4. Jeon do W, Chang BS, Jeung UO, Lee SJ, Lee CK, Kim MS, Nam WD. A case of postoperative tuberculous spondylitis with a bizarre course. Clin Orthop Surg. 2009 Mar;1(1):58-62..
5. Kaplan ES .Post-diskectomy tuberculous abscess. J Neurosurg 1973;38:358–361.
6. World Health Organization. Multidrug and extensively drug-resistant TB (M/XDR-TB): 2010 Global report on surveillance and response. 2010. Available at: http://www.who.int/tb/publications/2010/978924599191/en/ Accessed 25 Nov 2010.
7. World Health Organization. Guidelines for the programmatic management of drug-resistant tuberculosis. Emergency update 2008. 2008. Available at: http://www.who.int/tb/publications/2008/programmatic_guidelines_for_mdrtb/en/index.html Accessed 25 Nov 2010.
8. World Health Organization. Global tuberculosis control: a short update to the 2009 report. Available at: http://www.who.int/tb/publications/ global_report/2009/update/en/ Accessed 25 Nov 2010.
9. João Alves de Araújo-Filho, Arioldo Carvalho Vasconcelos-Jr, Eduardo Martins de Sousa, Colombina da Silveira, Elisangela Ribeiro, André Kipnis et al . Extensively Drug-Resistant Tuberculosis: A Case Report and Literature Review . BJID 2008; 12: 447- 452 .
10. Karen R. Jacobson, Dylan B. Tierney, Christie Y. Jeon, Carole D. Mitnick, Megan B. Murray. Treatment Outcomes among Patients with Extensively Drug-Resistant Tuberculosis:Systematic Review and Meta-Analysis . Clinical Infectious Diseases 2010; 51(1):6–14
11. Chee Kiang Phua, , Cynthia BE Chee, Angeline PG Chua, Suay Hong Gan, Aneez DB Ahmed, Yee Tang Wang . Managing a Case of Extensively Drug-Resistant (XDR) Pulmonary Tuberculosis in Singapore . Ann Acad Med Singapore 2011;40:132-5 .
12. Sapkas GS, Mavrogenis AF, Mastrokalos DS, Papadopoulos E, Papagelopoulos EC, Papagelopoulos PJ (2006) Postoperative spine infection: a retrospective analysis of 21 patients. Eur J Orthop Surg Traumatol 16(4):322–326.
| How to Cite this Article: Sonawane DV, Pawar E, Chandanwale A, Mathesul AA, Salunke A, Keny SM. Post-Operative Extensively Drug Resistant Mycobacterium Tuberculous Discitis. International Journal of Spine Apr – June 2016;1(1):47-49 . |