Volume 8 | Issue 2 | July-December 2023 | Page: 01-05 | Tushar V Soni, Sandip Singh, Manas Ranjan Deo, Varshesh Shah, Shreyansh Patel
DOI: https://doi.org/10.13107/ijs.2023.v08.i02.00
Submitted: 28/05/2023; Reviewed: 19/06/2023; Accepted: 05/11/2023; Published: 10/12/2023
Authors: Tushar V Soni [1], Sandip Singh [1], Manas Ranjan Deo [1], Varshesh Shah [1], Shreyansh Patel [1]
[1] Department of Neurosurgery, Smt. NHL MMC/ SVPIMSR, Ahmedabad, Gujarat, India.
Address of Correspondence
Dr. Sandip Singh,
Neurosurgery Resident, Department of Neurosurgery, Smt. NHL MMC/ SVPIMSR, Ahmedabad, Gujarat, India.
E-mail: dr.sandipsingh1100@gmail.com
Abstract
Background: Extramedullary teratoma in the spinal cord are very uncommon, especially in adults over 50 years of age, and more common in children, often with a history of spinal dysraphism.
Case Presentation: We report a rare case of a spinal intradural extramedullary mature cystic teratoma in a middle-aged adult located at the L1-L2 vertebral level with spinal dysraphism at a low sacral level and without any history of prior spinal procedures.
Discussion: Teratoma occurrences in the spine are extremely rare. Also, spinal intradural extramedullary teratoma is seen in children but is a rare entity in adults.
Conclusion: Although uncommon, spinal cord teratoma should be considered in the differential diagnosis of backache or radicular pain associated with neurological deficits even in absence of spinal dysraphism or any spinal procedure.
Keywords: Adults, Intradural extramedullary, Spinal, Teratoma
Introduction:
Extramedullary teratoma in the spinal cord are exceptionally rare, particularly among adults over 50 years of age. The incidence of intracranial teratoma is low, accounting for approximately 0.5–2.2% of all intracranial tumors[1]. Similarly, the occurrence of teratoma in the spine is extremely uncommon[2]. With the exception of the sacrococcygeal region, teratoma constitute less than 0.5% of all intraspinal tumors[3].
Case Report:
A 54-year-old adult male presented with complaints of difficulty walking persisting for one and a half years, accompanied by a gradual, progressive slippage of lower limb footwear over the past year. Additionally, he reported morning soiling of clothes occurring two to three times per week over the past year and pain in his right lower limb while walking for the last month. There was no history of spinal surgery or any other spinal procedures, such as lumbar puncture.
Physical examination revealed no dermal sinus tracts or cutaneous abnormalities. No congenital spinal deformities were observed. Neurological examination showed bilateral lower limb hypertonia and hyper-reflexia, no sensory deficit, bilateral lower limb power grade 5 on Medical Research Council (MRC) grading system at hip, knee, ankle and toes flexors and extensors except weakness in the left external hallucis longus (Power Grade 3 on MRC), bilateral plantar mute reflexes, and bowel-bladder incontinence. Laboratory parameters were unremarkable.
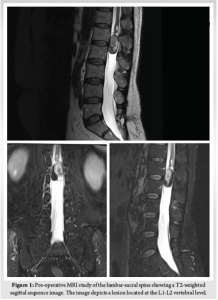
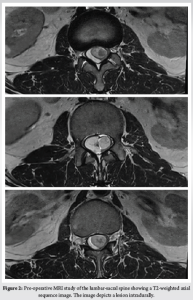
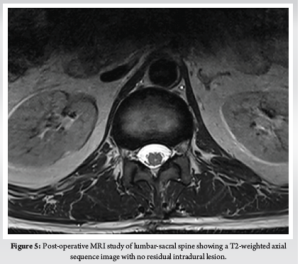
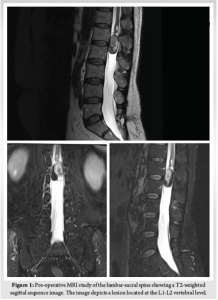
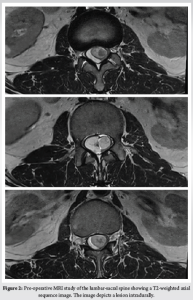
Magnetic resonance imaging (MRI) revealed a well-defined, non-enhancing intramedullary lesion measuring approximately 12x24x33mm (APxTRxCC) at the level of the conus, specifically at the L1-L2 vertebral level. The lesion appeared heterogeneous on T1-weighted images (hyperintense with internal hypointense solid component) and heterogeneous on T2-weighted images (iso to hyperintense with internal isointense solid component). Hyperintense components in T1-weighted images suggested the presence of internal fat components (Fig. 1, 2). No lateral extension of the lesion into the lateral recess was observed. Hypoplastic posterior elements were noted at the S1-S2 vertebral level, with unfused posterior elements observed at lower sacral vertebral levels. The rest of the spinal cord, cord termination, and conus medullaris appeared normal in intensity, with normal intervertebral discs and no prevertebral or paravertebral collections.
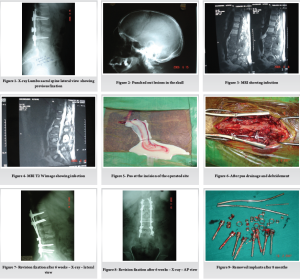
Elective surgical intervention was planned, and the patient underwent L1-L2 laminectomy with total resection of the tumor while in the prone position. The dura mater was exposed well and opened via a midline incision. Intraoperative findings suggested the presence of an intradural extramedullary yellowish cyst. The tumor capsule was separated, and total removal of the tumor was achieved. The dura was closed in a watertight manner. Upon incision into the tumor tissue, whitish fluid containing grayish soft tumor tissue was found.
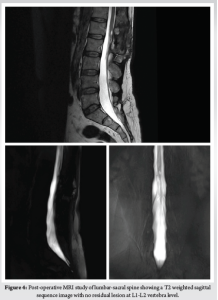
The postoperative period was uneventful, and the patient was discharged on post-operative day 5 without any neurological deficits or signs of meningitis. Neurological examination at discharge revealed bilateral lower limb normal tone and deep tendon reflex 2+ , no sensory deficit, bilateral lower limb power grade 5 on Medical Research Council (MRC) grading system at hip, knee, ankle and toes flexors and extensors with persistent weakness in the left external hallucis longus (Power Grade 3 on MRC), bilateral plantar downgoing reflexes, and improved bowel-bladder incontinence. No neurological deterioration was observed during the 2-month follow-up period.
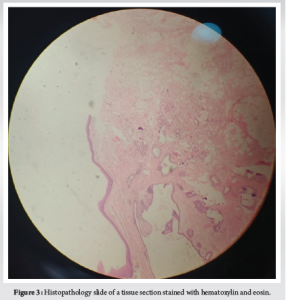
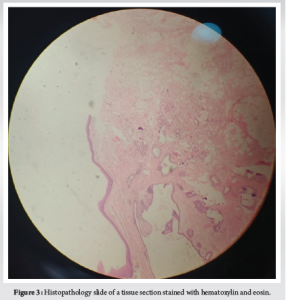
Histopathological analysis indicated features suggestive of a mature cystic teratoma, including stratified squamous epithelium, transitional epithelium, adnexal structures (sebaceous glands, sweat glands), mature adipose tissue, muscle tissue, glial tissue, respiratory-type mucosal glands, blood vessels, and keratin-like flakes (Fig. 3).
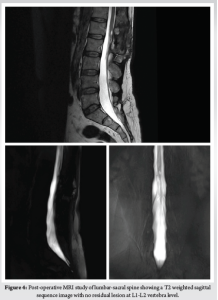
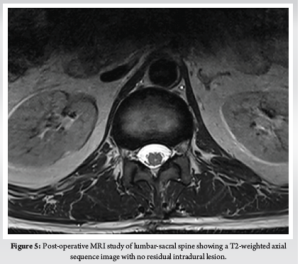
Follow-up MRI scans showed no residual or new lesions (Fig. 4, 5).
Discussion:
The spinal teratoma is an uncommon condition. The first documented case of this ailment was presented by Virchow in 1863 [5], followed by another case reported by Gowers and Horsley 25 years later [6]. Medical literature contains only a limited number of studies on this subject. Spinal intradural extramedullary teratoma is infrequent among adults but is more commonly observed in children and is often linked with spinal dysraphism [7]. Various spinal malformations such as spina bifida, partial sacral agenesis, tethered cord syndrome, hemivertebrae, myelomeningocele, and diastematomyelia have been associated with teratoma in the literature [8-12]. Apart from congenital abnormalities, instances have been documented where trauma or surgical procedures (e.g., lumbar puncture) have preceded the onset of symptoms in adults [13, 14]. Iatrogenic cysts may develop due to the introduction of epithelial cells during epidural spinal injections or the inclusion of dermal or epidermal tissue during the closure of a myelomeningocele [15]. Epidermoid and dermoid cysts, accounting for less than 1% of spinal tumors, can be either congenital or iatrogenic [16]. We presented a rare case of spinal intradural extramedullary cystic teratoma in a middle-aged adult with spinal dysraphism at the sacral level without any prior history of spinal procedures.
Numerous researchers have indicated that the thoracolumbar region, particularly around the conus medullaris, is frequently affected [8-10]. Clinical manifestations such as leg weakness, sensory alterations, and reflex abnormalities are closely associated with the tumor’s location [10]. In the literature, the majority of cases have presented with these symptoms [8-11, 14]. Our case was consistent with these findings regarding the clinical features of the tumor. Operative findings revealed severe compression of the spinal cord by the mass. However, the patient did not exhibit severe neurological symptoms, possibly due to the slow-growing nature of the tumor.
MRI findings typically indicate intradural extramedullary tumors, leading to the widening of the cerebrospinal fluid space above and below the tumor, alongside displacement of the cord to the contralateral side of the thecal sac, and a clear demarcation between the tumor and cerebrospinal fluid. Larger tumors often result in the flattening of the spinal cord against the dura mater on the contralateral side [16]. In our case, the MRI scan depicted a distinct intradural extramedullary mass lesion, primarily localized opposite the L1-L2 vertebrae level on the right side. This lesion compressed and displaced the caudaequina nerve roots, thereby explaining the progressive sensory symptoms experienced by the patient. MRI serves as the gold standard diagnostic tool for identifying teratoma and assessing the extent of spinal cord involvement [7]. However, preoperative diagnosis of spinal teratoma remains challenging, as MRI features cannot definitively differentiate between teratoma and other extramedullary lesions [17]. Ultimately, histopathological examination following surgery is essential to confirm the diagnosis of an intraspinal mature teratoma [18].
The diagnosis of teratoma relies on histopathological identification, confirming the presence of tissues representing the three germinal layers: ectoderm, mesoderm, and endoderm [19]. However, the absence of one germinal layer does not necessarily exclude the diagnosis [10]. Li et al.’s analysis of the literature suggested that in several cases, only two of the three germinal layers were observable. This observation was attributed to the growth of derivatives from one or two layers over the others [10, 20, 21].
Two prevailing theories explain the origin of intraspinal teratoma: the dysembryogenic theory and the misplaced germ cell theory [25, 26]. According to the dysembryogenic theory, spinal teratoma develop from pluripotent cells. In a locally disrupted developmental environment, these cells undergo incoherent differentiation, leading to the formation of a spinal teratoma. Such disordered development typically occurs in a primitive streak or a caudal cell mass [23, 27]. The misplaced germ cell theory posits that certain pluripotent primordial germ cells of the neural tube become displaced during migration from the yolk sac to the gonad, resulting in the formation of spinal teratoma [26]. In adult intraspinal teratoma, which seldom present with significant dysraphism, the misplaced germ cell theory is considered more plausible [8, 18, 25, 28, 29]. The presence of a mature teratoma in our case may lend support to the notion of a tumor originating from misplaced pluripotent primordial germ cells.
The preferred treatment for symptomatic patients is total surgical excision of the lesion. However, in approximately 50% of cases, intimal adhesion of the teratoma to the surrounding neural parenchyma complicates total tumor resection [8, 9, 10, 22]. Subtotal resection increases the risk of recurrence, as reported by several authors. Therefore, they recommend excising the tumor as extensively as possible while preserving all surrounding neural tissue[9,10,14]. Additionally, it is crucial not to spill the cystic contents into the intradural space during surgery, as this can lead to the development of aseptic chemical meningitis with or without obstructive hydrocephalus [13, 14, 23]. The role of adjuvant therapies, including radiotherapy and chemotherapy for remnant tumors, has not been clearly characterized [9]. Furthermore, the effects of these therapies on immature and malignant teratoma remain disputed [22, 24].
Conclusion: Intradural extramedullary teratoma is an uncommon tumor. We present a rare case of a spinal intradural extramedullary mature cystic teratoma in a middle-aged adult. In our case, we performed a near-total removal due to severe adhesion of the teratomas to the surrounding normal tissue. Intraoperative findings and histopathological examination confirm the diagnosis. Surgical excision should be considered the treatment of choice for symptomatic lesions. Recurrence, if any, of the tumor will be ruled out on long-term follow-up.
References
1. Pandey S, Sharma V, Shinde N, Ghosh A. Spinal intradural extramedullary mature cystic teratoma in an adult: A rare tumor with review of literature. Asian Journal of Neurosurgery. 2015 Sep;10(03):133-7.
2. Cybulski GR, Von Roenn KA, Bailey OT. Intramedullary cystic teratoid tumor of the cervical spinal cord in association with a teratoma of the ovary. Surg Neurol 1984;22:267-72.
3. ElmaciI, DagcinarA, Ozgen S, Ekinci G, Pamir MN. Diastematomyelia and spinal teratoma in an adult. Case report. Neurosurg Focus 2001;10:ecp2.
4. Borlot F, Soares MS, Espíndola AA, Reed UC, Matushita H, Teixeira MJ. Intramedullary spinal teratoma a rare condition with a good outcome. Arq Neuropsiquiatr 2009;67:733-5.
5. Hejazi N, Wizmann A : Spinal intramedullary teratoma with exophytic components : report of two cases and review of the literature. Neurosur Rev 26 : 113-116, 2003.
6. Poeze M, Herpers M, Tjandra B, Freling G, Beuls E : Intramedullary spinal teratoma presenting with urinary retension : case report and review of the literature. Neurosurgery 45 : 379-385, 1999.
7. Sung KS, Sung SK, Choi HJ, SongYJ. Spinal intradural extramedullary mature cystic teratoma in an adult. J Korean Neurosurg Soc 2008;44:334-7.
8. Ak H, Ulu MO, Sar M, Albayram S, Aydin S, Uzan M. Adult intramedullary mature teratoma of the spinal cord: Review of the literature illustrated with an unusual example. Acta Neurochir (Wien) 2006;148:663-9.
9. Makary R, Wolfson D, Dasilva V, Mohammadi A, Shuja S. Intramedullary mature teratoma of the cervical spinal cord at C1-2 associated with occult spinal dysraphism in an adult. Case report and review of the literature. J Neurosurg Spine 2007;6:579-84.
10. Nonomura Y, Miyamoto K, Wada E, Hosoe H, Nishimoto H, Ogura H, et al. Intramedullary teratoma of the spine: Report of two adult cases. Spinal Cord 2002;40:40-3.
11. Poeze M, Herpers MJ, Tjandra B, Freling G, Beuls EA. Intramedullary spinal teratoma presenting with urinary retention: Case report and review of the literature. Neurosurgery 1999;45:379-85.
12. Güvenç BH, Etus V, Muezzinoglu B. Lumbar teratoma presenting intradural and extramedullary extension in a neonate. Spine J 2006;6:90-3.
13. Cavazzani P, Ruelle A, Michelozzi G, Andrioli G. Spinal dermoid cysts originating intracranial fat drops causing obstructive hydrocephalus: Case reports. Surg Neurol 1995;43:466-9.
14. Stevens QE, Kattner KA, Chen YH, Rahman MA. Intradural extramedullary mature cystic teratoma: Not only a childhood disease. J Spinal Disord Tech 2006;19:213-6. Stevens QE, Kattner KA, Chen YH, Rahman MA. Intradural extramedullary mature cystic teratoma: Not only a childhood disease. J Spinal Disord Tech 2006;19:213-6.
15. Kudo N, Hasegawa K, Ogose A, Hotta T, Watanabe K, Tojo T, et al. Malignant transformation of a lumbar intradural dermoid cyst. J Orthop Sci 2007;12:300-2.
16. Gebauer GP, Farjoodi P, Sciubba DM, Gokaslan ZL, Riley LH 3rd, Wasserman BA, et al. Magnetic resonance imaging of spine tumors: Classification, differential diagnosis, and spectrum of disease. J Bone Joint Surg Am 2008;90 Suppl 4:146-62.
17. Virchow R. Die krankhaften Geschwulste. Dreissing Vorlesungen gehalten wahrend des Wintersemesters 1862-1867 an der Universitat zu Berlin. Vol 1-3. Berlin, Germany: A. Hirschwald;1863-5.
18. Sharma MC, Aggarwal M, Ralte AM, Vaishya V, Suri A, Gupta V, et al. Clinicopathological study of spinal teratomas. A series of 10 case. J Neurosurg Sci 2003;47:95-100.
19. Tapper D, Lack EE. Teratomas in infancy and childhood. A 54-year experience at the Children’s Hospital Medical Center. Ann Surg 1983;198:398-410.
20. Li Y, Yang B, Song L, Yan D. Mature teratoma of the spinal cord in adults: An unusual case. Oncol Lett 2013;6:942-46.
21. Rosenbaum TJ, Soule EH, Onofrio BM. Teratomatous cyst of the spinal canal. Case report. J Neurosurg 1978;49:292-7.
22. . Allsopp G, Sgouros S, Barber P, Walsh AR : Spinal teratoma : is there a place for adjuvant treatment? Two case and a review of the literature. Br J Neurosurg 14 : 482-488, 2000.
23. Koen JL, McLendon RE, George TM : Intradural spinal teratoma : evidence for a dysembryogenic origin. J Neurosurg 89 : 844-851, 1998.
24. Fernandez-Cornejo VJ, Martinez-Perez M, Polo-Garcia LA, MartinezLage JF, et al : Cystic mature teratoma of the filum terminale in an adult. Case report and review of the literature. Neurocirugia (Astur) 15 : 290-293, 2004.
25. Al-Sarraj ST, Parmar D, Dean AF, Phookun G, Bridges LR. Clinicopathological study of seven cases of spinal cord teratoma: A possible germ cell origin. Histopathology 1998;32:51-6.
26. Rewcastle NB, Francoeur J. Teratomatous cysts of the spinal canal; with “sex chromatin” studies. Arch Neurol 1964;11:91-9.
27. Reddy CR, Rao KV, Jagabhandhu N. Intraspinal teratoma associated with diastematomyelia. Indian J Pathol Bacteriol 1968;11:77-81.
28. Jian W, Ying W, Chao Y. Intramedullary spinal teratoma of the conus medullaris: Report of two cases. Acta Neurochir (Wien) 2010;152:553-4.
29. Sharma MC, Jain D, Sarkar C, Suri V, Garg A, Singh M, et al. Spinal teratomas: A clinico-pathological study of 27 patients. Acta Neurochir (Wien) 2009;151:245-52.
How to Cite this Article: Soni TV, Singh S, Deo MR, Shah V, Patel S| Rare Case of Spinal Intradural Extramedullary Mature Cystic Teratoma in a Middle Aged Adult| International Journal of Spine| July-December 2023; 8(2): 01-05.
|