Treatment Algorithm For Unstable Burst Fracture
Volume 1 | Issue 2 | Sep – Dec 2016 | Page 27-32 | Ketan Khurjekar, Himanshu Kulkarni, Mayur Kardile
Authors : Ketan Khurjekar [1], Himanshu Kulkarni [1], Mayur Kardile1 [1]
[1] Department of Spine Surgery, Sancheti Institute for Orthopaedics and Rehabilitation, Pune India
Address of Correspondence
Dr. Ketan Khurjekar
Department of Spine Surgery, Sancheti Institute for Orthopaedics and Rehabilitation, Pune India
Email : kkhurjekar@gmail.com
Introduction
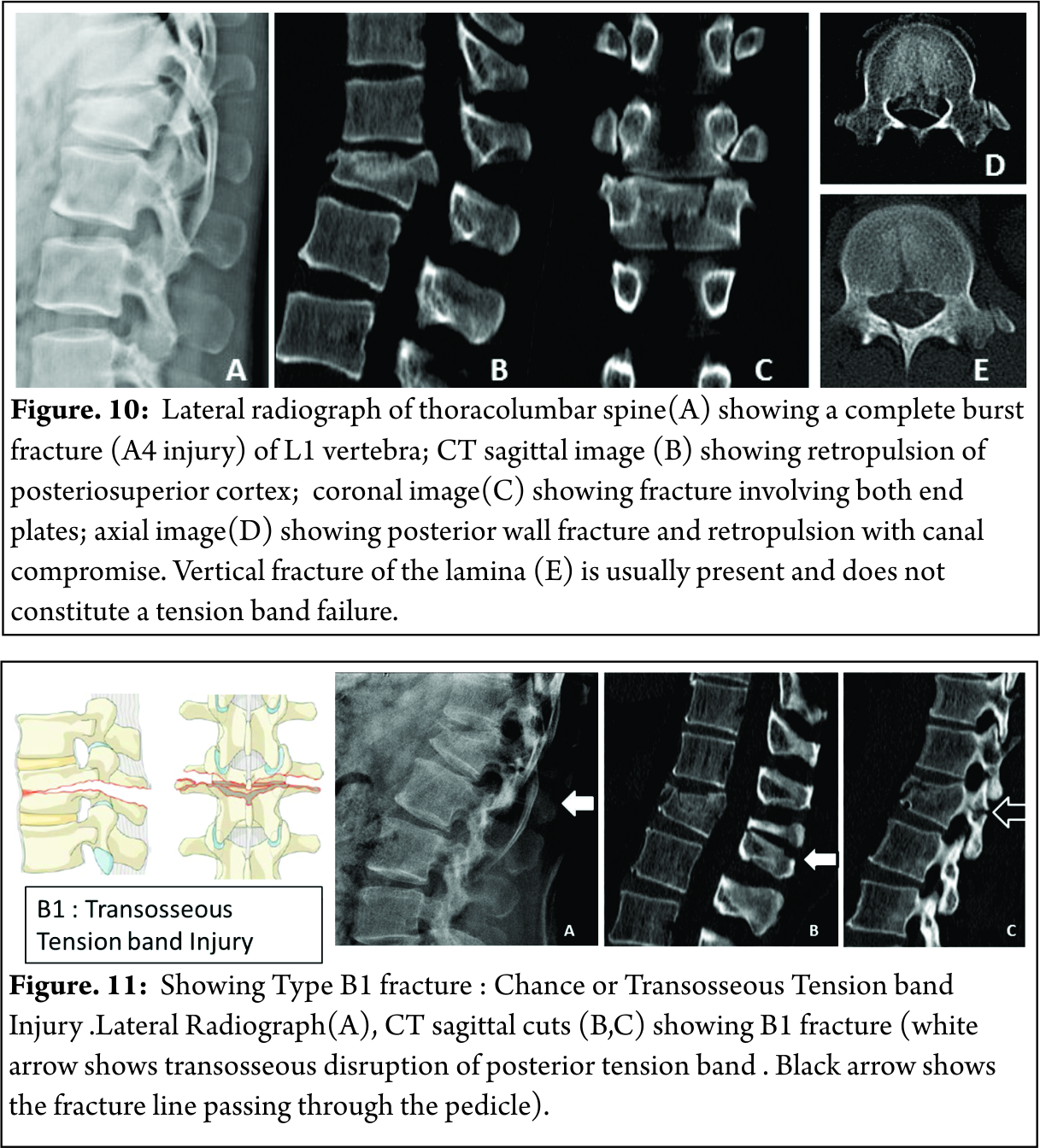
Burst fractures comprise of approximately 17% of all thoracolumbar fractures. These type of fractures result from compression failure of both the anterior and middle columns under substantial axial loads [1]. Between the immobile, kyphotic thoracic spine above, and the relatively mobile, lordotic lumbar spine below, throracolumbar region makes a transition zone where all the stress forces are concentrated. This makes the thoraco lumbar zone more prone to injuries than any other part of the spinal column. According to Denis, a spinal fracture is described as burst if there is compression of the anterior column, fracture of the middle column, and retropulsion of bone fragments into the spinal canal [2]. As a result neurologic injury has been reported to occur in 30% of the patients with thoracolumbar fractures [3]. The management of thoracolumbar burst fractures remains challenging. An ideal treatment modality should induce neurological recovery, should correct the deformity efficiently and allow early mobilization, should enable minimization of loss of work hours and should have minimal treatment related complications. For years together, a lot has been written in literature about how these aims can be achieved, with strong proponents for both non-operative and operative treatments existing. This difference of opinion and polarising philosophies can be confusing for an inexperienced clinician. So we have tried to put forth step by step approach to decode the dilemma that is the unstable thoracolumbar burst fracture with the help of a case.
Case-
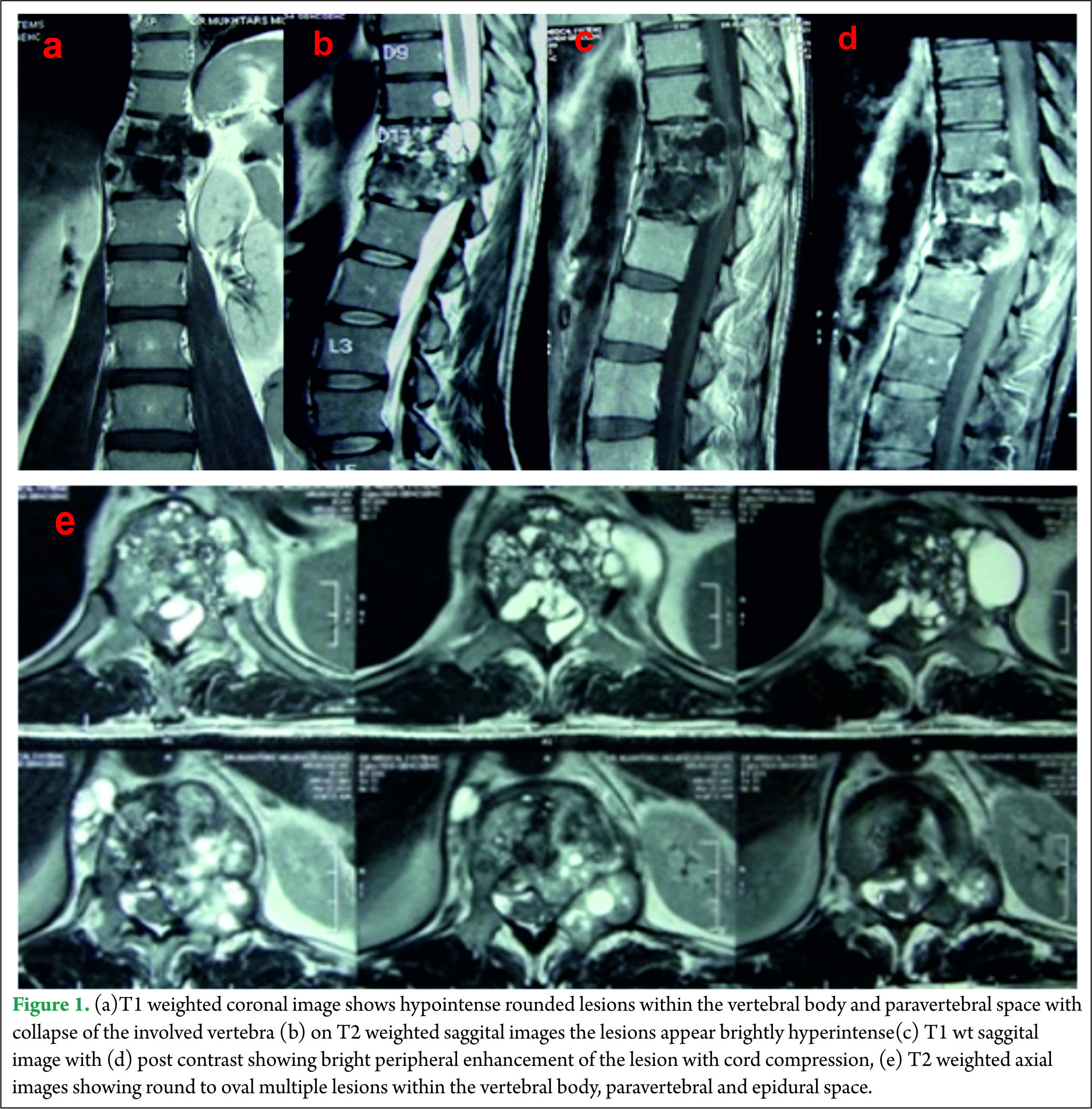
A 21 year old engineering student came to casualty with history of fall from height 4 hours back. Patient was unable to move both his lower limbs. Power in both Hips wad grade 2 for flexion, Grade 1 for Knee extension and Grade 0 for ankle and great toe movements. There was partial loss of sensations with diminished sensations present in L1-2-3 dermatomes and complete loss of sensations below that. There was loss of sensation for micturition, but it was associated with weak anal contraction. Patient was shifted to department of radiology and plane radiogram was done. Plain lateral radiogram showed fracture of L2 vertebral body with a retropulsed fragment crossing posterior vertebral line (Fig. 1).

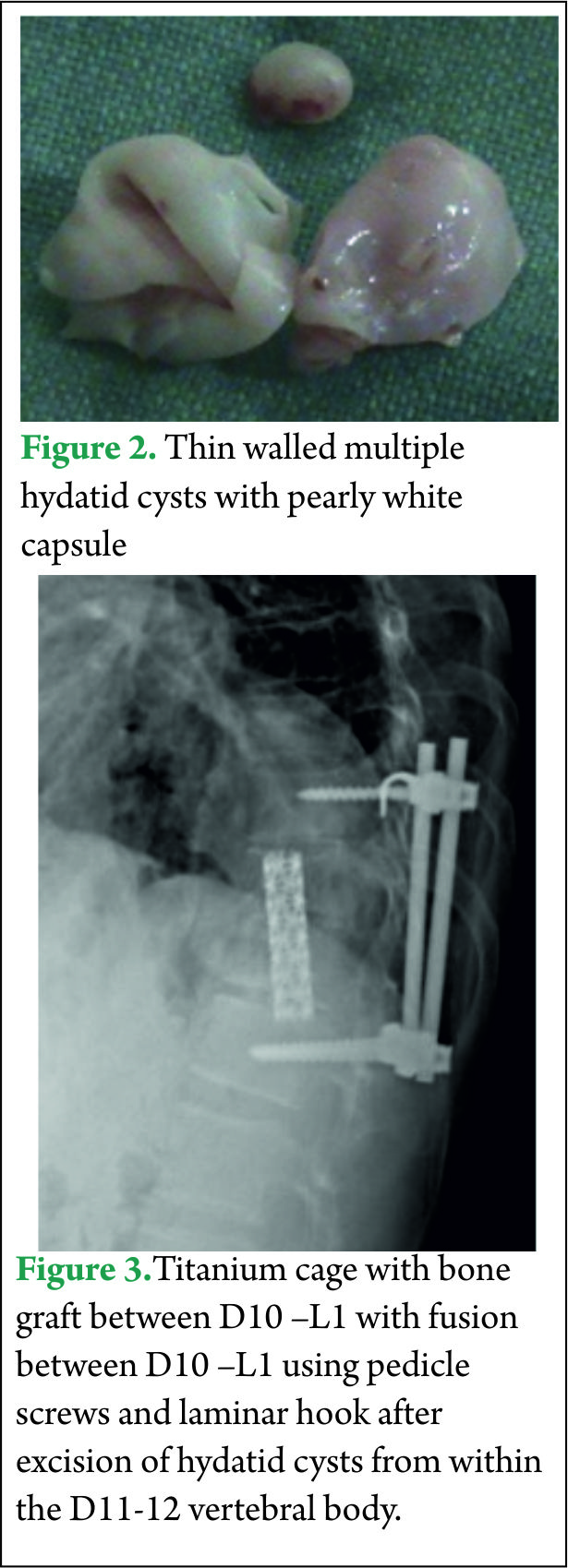
After this, MRI scan of the thoracolumbar spine was done. The scan showed the retropulsed fragments causing severe compression of the cord (Fig. 2).
Once the imaging studies were done, following steps were followed.
Assesment of Neurology –
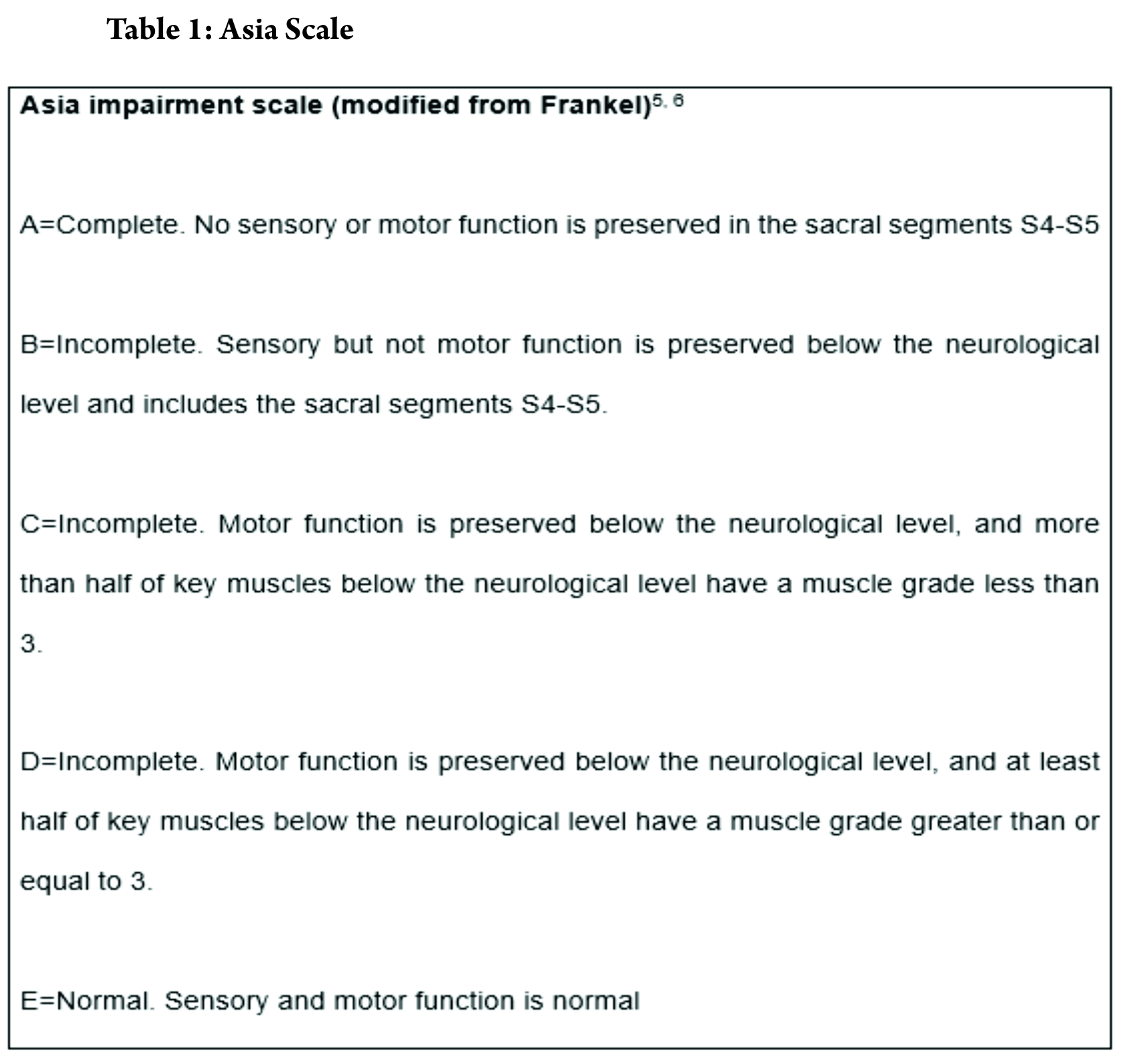
Assessment of neurology has to be the first thing to be considered in a methodical treatment approach. In most circumstances, the treatment protocol and prognosis depends upon early neurological state. Frankel categorised the spinal cord injuries in a comprehensive classification. The injury was divided into 5 types, from severe to less severe. Modification of Frankel grading was included in now widely accepted American Spine Injury Association grading (ASIA Grading) in 1997 which was revised in 2011 [4]. ASIA grading grades the injury into complete or incomplete, with extensive dermatomal and myotomal charting.
Power charting for upper and lower limb myotomes was done. According to Frankel grading, the injury was labelled as Frankel 3, since some voluntary motor function was preserved below level of lesion but too was weak to serve any useful purpose. Some sensations were preserved too.
Assessment of stability-
In 1949, Nicoll [7] first introduced the concept of posttraumatic spinal instability. He defined unstable spinal injuries based on the presence of subluxation or dislocation, disruption of interspinal ligaments, or laminar fractures at L4 or L5. This concept has been used as a base for all the treatment approaches for unstable injures. It was stated by White and Panjabi that a stable spine is able, under physiological load, to maintain its normal movement so that there is no initial or additional neurological deficit, no major deformity, and no incapacitating pain.8 They also made a check list for thoracic instability.
According to Denis [2], there are 3 types of instability in the thoracolumbar spine; the mechanical instability that refers to the potential of spinal collapse with subsequent deformity, the neurological instability that refers to the potential of further neurological injury, and the combined mechanical and neurologic instability. The 3-column model is useful for the assessment of spinal instability; any thoracolumbar burst fracture can be unstable, while middle 2, or 2-column failures are absolute criteria for instability.
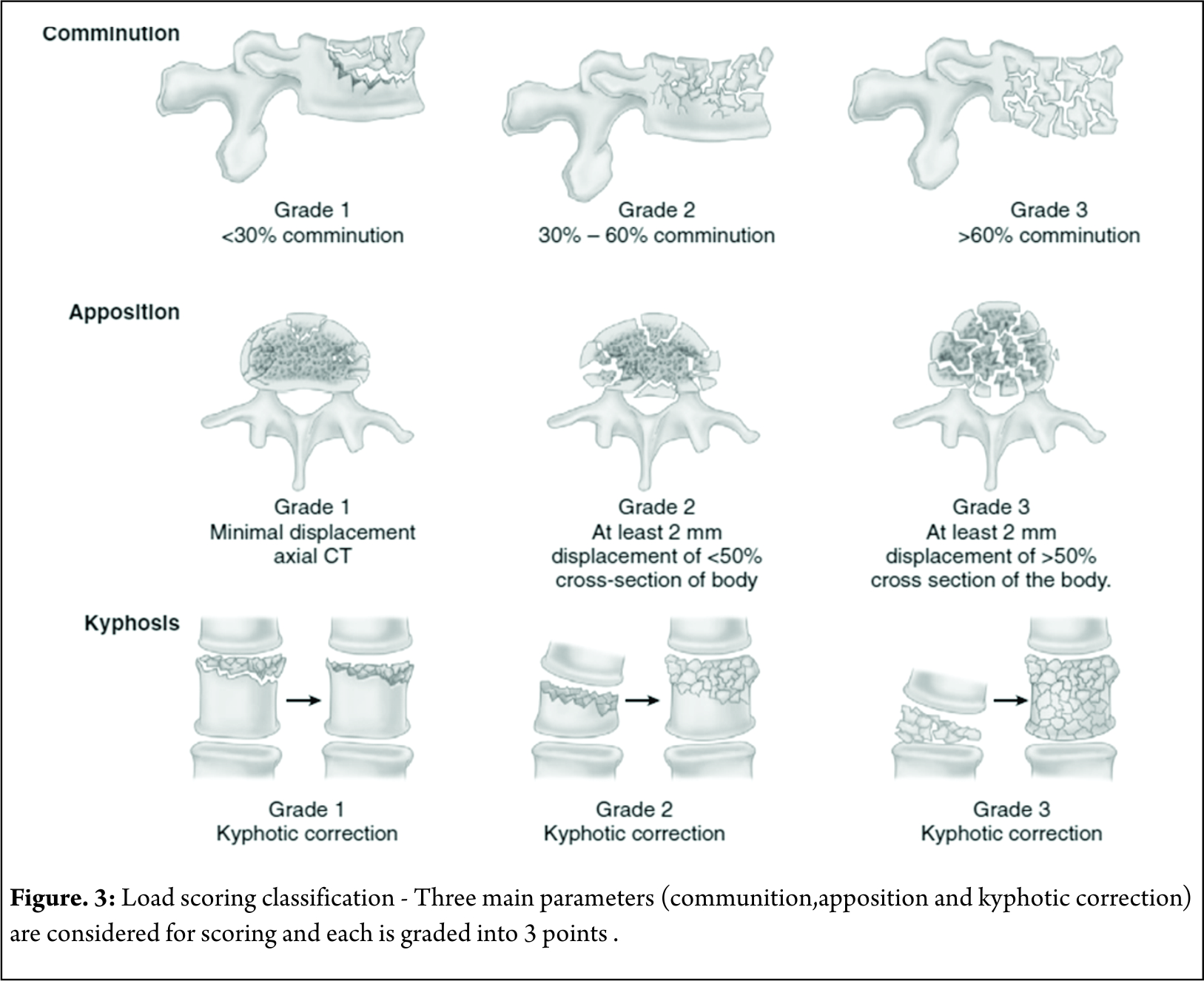
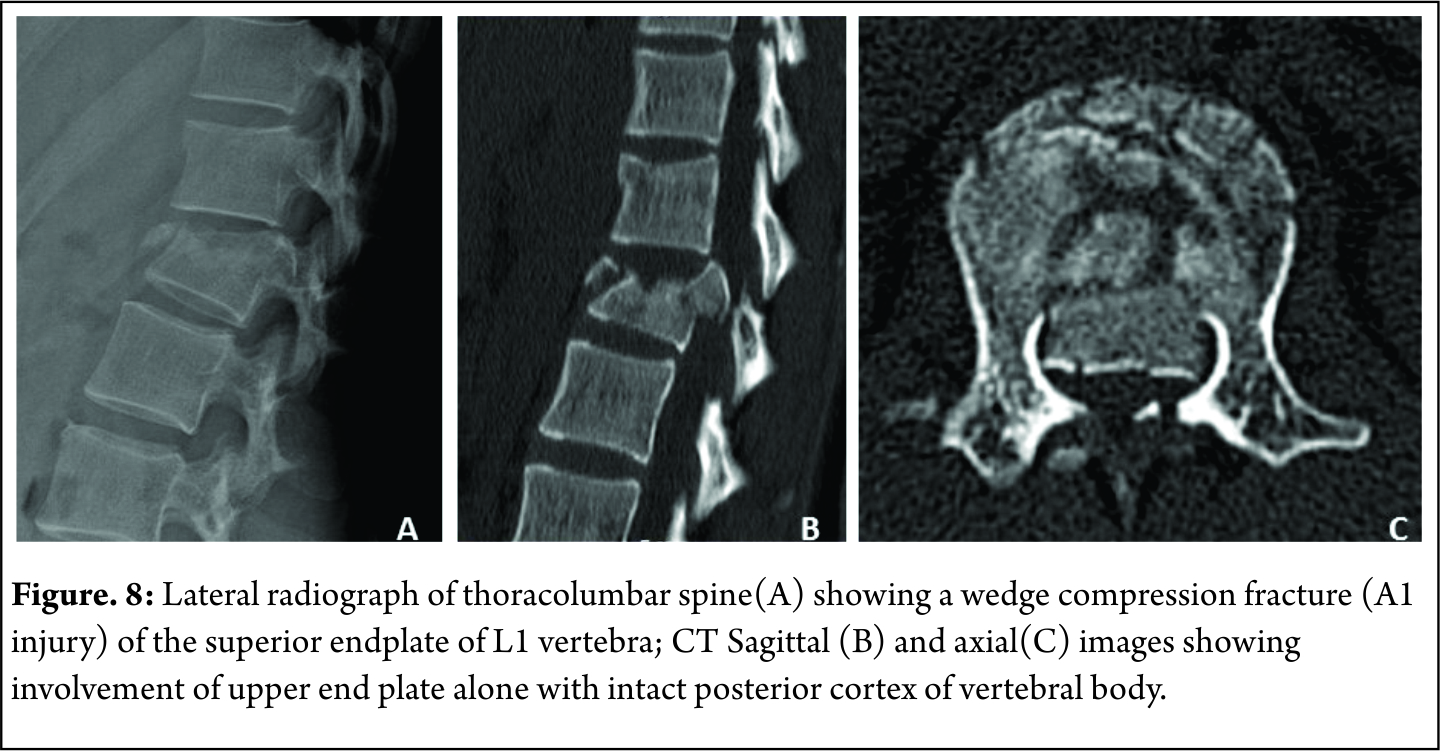
Mcafee et al in 1984 described factors indicative of instability in compression burst fractures of thoracic lumbar junction. According this criteria, fracture in our case was considered unstable. The fracture had progressive neurological deficit, had >50% loss of vertebral height, local kyphosis > 20 degrees and retropulsion of a bony fragment in the canal was present (Fig. 3).
Classifying the fracture pattern –
Since Bohler first tried to classify thoracolumbar spine fractures combining both anatomic appearance and mechanisms of injury as early as in 1930, classification of spinal fractures to facilitate communication and encourage optimal treatment protocols has long been a focus of the spine community [9]. Numerous classification systems have been put forth till now. Discussion of all is beyond the scope of this topic but none has been proven to be a gold standard yet due to the complexity of spinal anatomy and mechanisms of injury, as well as widely differing philosophies in treatment[10].
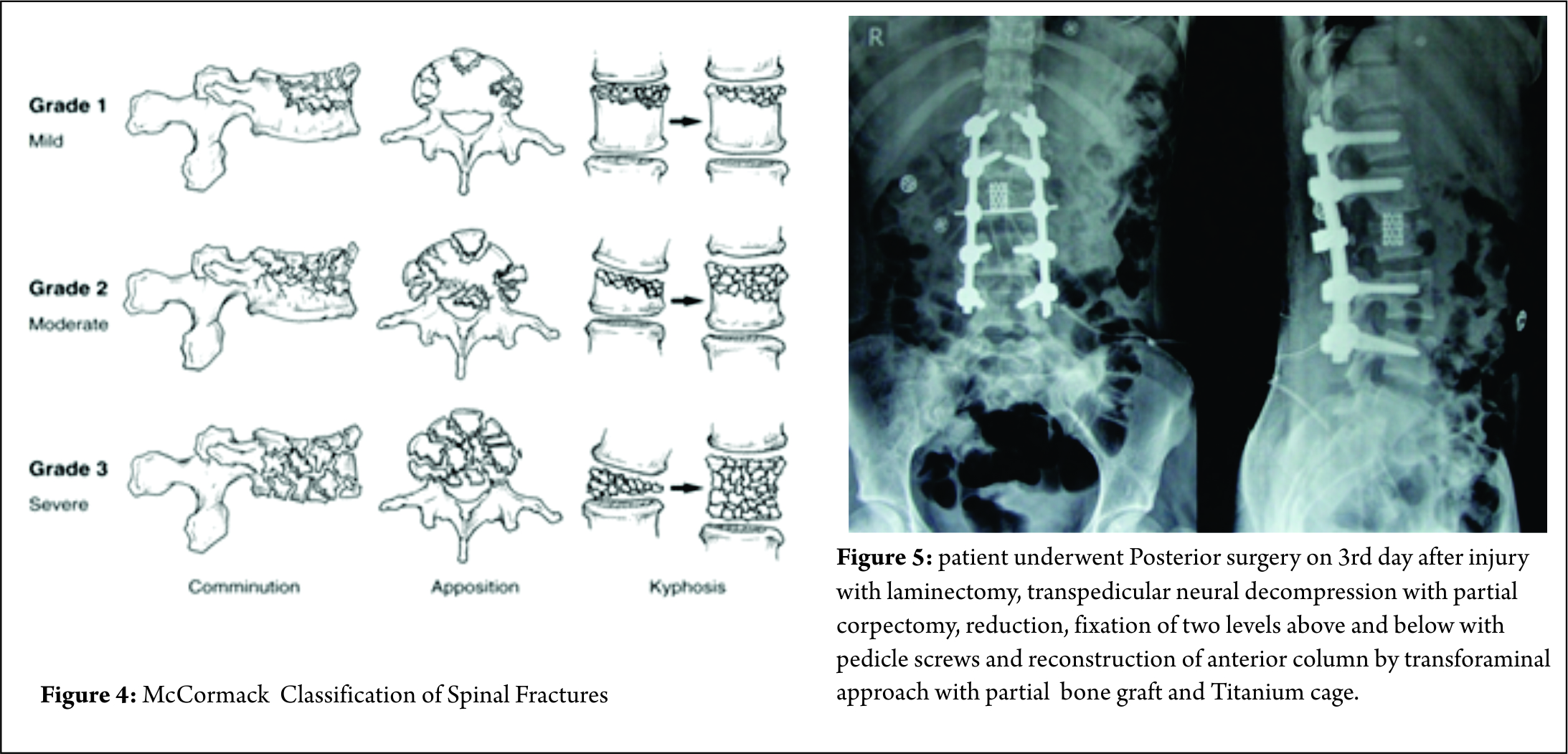
Some classification systems have gained more acceptance than others though. In 1994, McCormack et al [11]. stated that in long bone fixation, load sharing between the bone and the implant is of paramount importance. It helps in uneventful healing of the fracture and prevents implant failure. They applied same concept in spinal fractures, and put forth a CT based Load sharing classification taking into account the amount of comminution, apposition and Kyphosis.
The fracture in this case was classified as a Grade 2, with moderate comminution (Fig. 4) apposition and Kyphosis. Fracture was also classified according to Thoracolumbar injury classification and severity score (TICS) which is useful guide to treatment options. The classification holds a scoring system categorising the injury into operative or non-operative category based on the score.
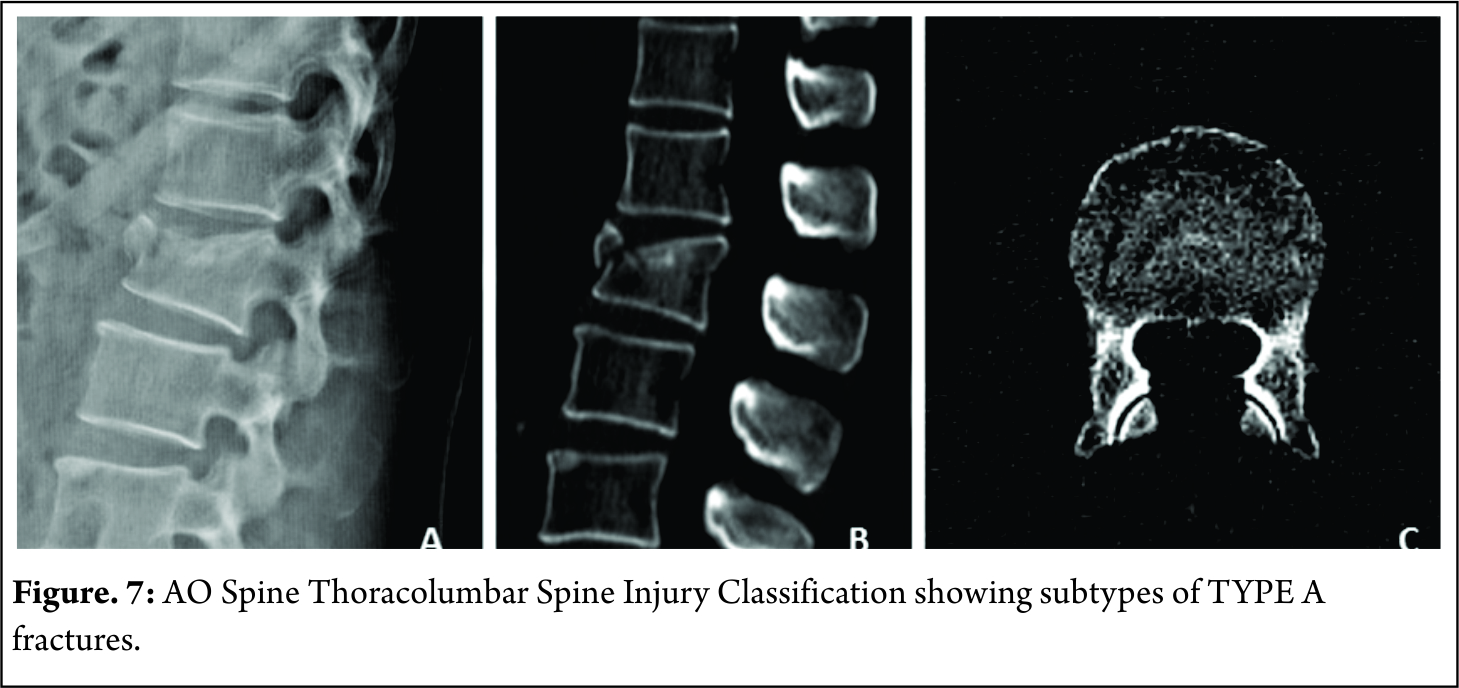
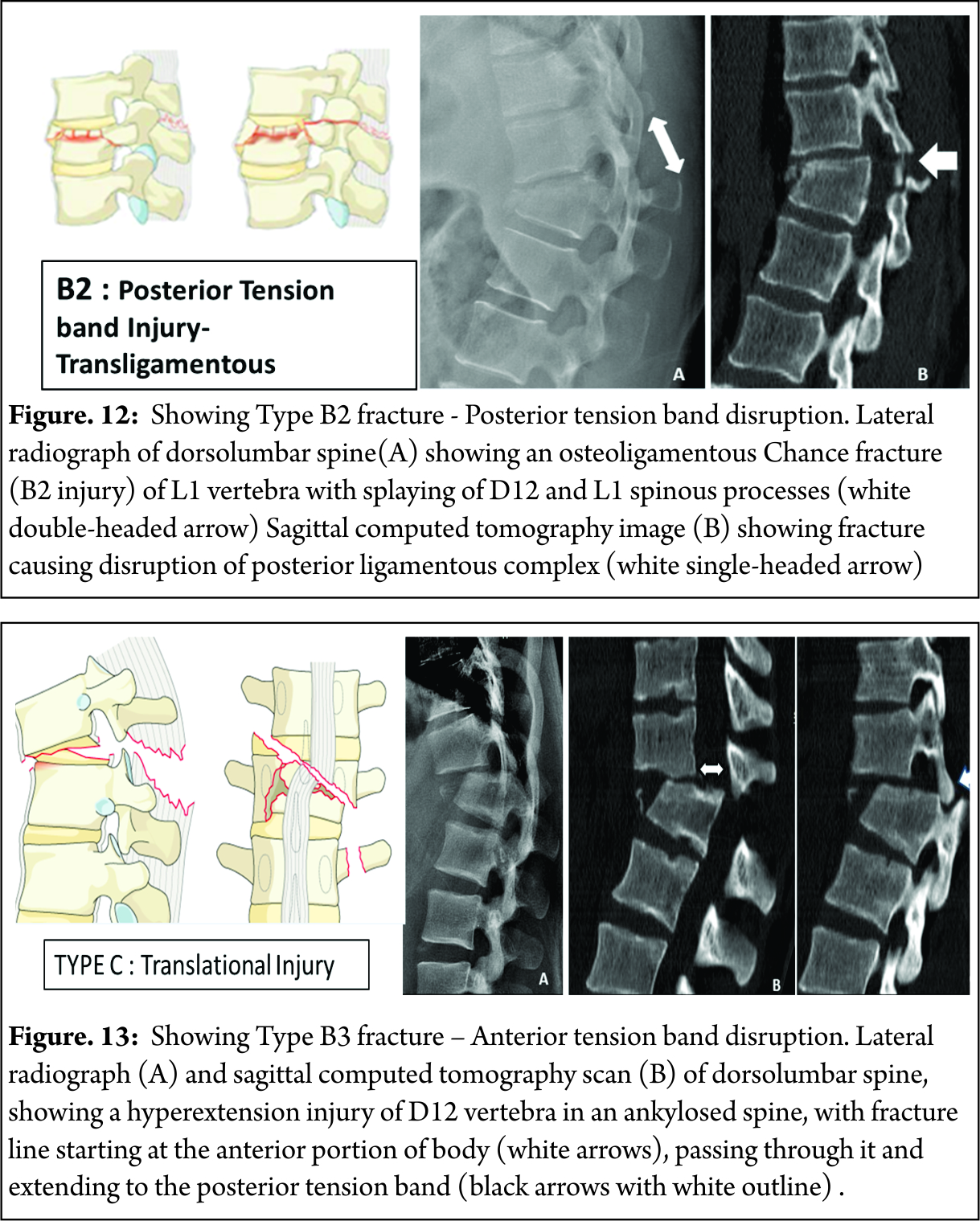
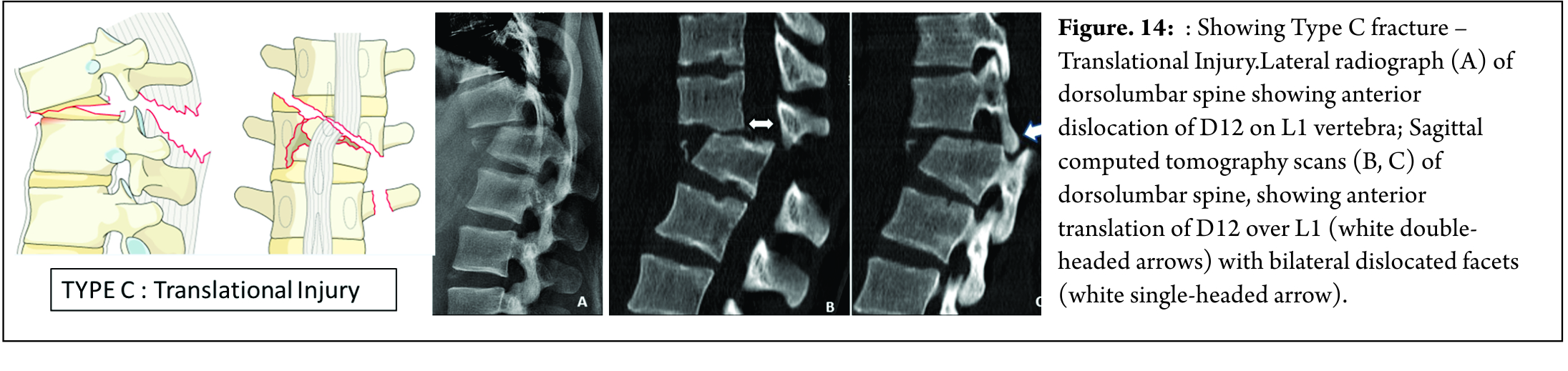
The score for our fracture was found to be 8, which indicated the management should be operative. Like other long bone fractures, AO classification was also introduced in as AO- Magerl classification [12]. The classification system failed to gain wide universal international adoption due to its complexity. SO, the system was revised in 2013 into 3 main injury patterns: type A (compression), type B (tension band disruption), and type C (displacement/translation) injuries[13].
Our facture was classified as L2-B2;N3;M1.
Management Options –
Ideally, the treatment Goal in burst fracture should be to
1. Effective correction the deformity
2. Induction neurological recovery
3. Should allow early mobilization
4. Should have minimal risk of complication
Because of different philosophical ideologies, and there has been considerable controversy on the efficacy of conservative treatment and the need for surgical intervention in burst fractures with intact neuro status.
Argument for proponents of Surgery has always been on points of additional stability, prevention of neurological deterioration, attainment of canal clearance, prevention of kyphosis and early relief of pain. Denis et al [2]. reported late neurological deterioration in 17% of conservatively treated patients. They stated that prophylactic stabilization and fusion of acute burst fractures without neurologic deficit have significant advantages over conservative treatment. Likewise, Bohlman et al too were biased towards operative intervention. They expressed that operative intervention enhances clinical outcome and facilitates early rehabilitation [14]. However, Many subsequent trials showed that deterioration of the neurological status in patents who had intact neurology initially was unlikely [15,16]. To comment about the concerns about the persistent canal compromise in neurologically intact patients, Shen et al [17]. noted a resorption of approximately 50% of the retroplused fragment within 12 months. Also, no statistical difference was found in the degree of spinal canal remodelling between patients treated conservatively and operatively [18]. Also, Some surgeons have chosen direct decompression and canal clearance when CT scan has showed more than 40 % canal compromise [19]. However paralysis occurs at the moment of injury and it is not related to position of bony fragment [26]. Also, High-speed video tests have shown that at higher levels of occlusion, the final position of the bone fragments was inadequately correlated with the maximum level of impingement [27].
So, even though the preferred treatment for these fractures with intact neurology is still an ongoing debate amongst clinician, data has shown no significant superiority of operative treatment over non operative treatment. TLICS is a useful tool to make the decision of preferred treatment modality easy.
In patients with progressive neurological deterioration, or ones with unstable fractures & complete neurological loss, there’s no debate about the choice of surgical intervention as a preferred treatment modality. It ensures decompression of the spinal canal and nerve roots, and gives the fractured spine sufficient stability and realignment with correction of kyphosis to start early mobilization and rehabilitation [14]. Timing of the surgery is also a debatable factor. It’s a common opinion that surgery at the earliest can be beneficial for ultimate outcome. Carlo Bellabarba et al in 2010 stated that stabilization within 72 hours was safe and decreased respiratory morbidity. But other than decreased ICU and overall hospital stay, no other significant benefit of early surgery was found. It was also stated that currently there is very low supporting evidence in literature for benefits early surgery [19]. Surgery for these fractures can be via Anterior, posterior or a combined approach. Fracture morphology, neurologic status, and surgeon preference play major roles in making the decision about preferred approach. Usually, the anterior approach surgery should be limitedly used for severe Denis type B fracture with direct reduction. The posterior approach is used in most Denis type A and B fractures with indirect reduction and has less complication [20]. Some authors also stated that anterior only showed statistically significant improvement in sagittal alignment in long term follow up than posterior only fixation [21]. Anterior and middle column injuries with partial neurology have been effectively treated by anterior approach; decompression under direct vision and sagittal alignment are the key factor.
In our experience, anterior decompression and reconstruction for burst fractures with anterior and median column injury is effective. Decompression and reconstruction can be performed under direct vision at one stage, and the sagittal alignment can be corrected at the same time. Since anterior approach has a more surgical morbidity than posterior approach, it should be reserved for patients with canal compromise >67%. Focal kyphosis > 30 degree [22].
But at the same time, The benefits of posterior approach cant be undermined. It is more than once described that creating a posterior tension band and stabilisation is biomechanicvally more stronger It helps in Indirect decompression by ligamentotaxis ( though, ligamentotaxis has been shown to be inefficient in greater than 50% canal compromise 22), direct access to spinal canal for decompression, relieve hematoma, repair dural tears and extricate trapped nerve roots. Direct canal decompression through a posterior approach can be obtained by laminectomy, pediculectomy, fragment reposition or fragment removal [23]. Also, adequate neural canal decompression can also be achieved by a new modified transpedicular approach less invasively to avoid anterior surgery [24]. Kaya et al extended the transpedicular decompression for spinal cord and nerves by posterior alone approach along with stabilisation and showed adequately good results for burst fracture (spine J 2004) In posterior approach, the extent of fixation should be decided according to the classification of the fracture. Short segment fixation could usually suffice in AO type A and B fractures. Long segment fixations should be carried out in AO type 3 fractures, severely comminuted fractures and osteoporotic bones [25]. We feel that incomplete neurological deficit with demonstrable radiological compression on MRI, should be subjected to canal clearance either by transpedicular approach or direct decompression, anteriorly or posteriorly. So patient underwent Posterior surgery on 3rd day after injury with laminectomy, transpedicular neural decompression with partial corpectomy, reduction, fixation of two levels above and below with pedicle screws and reconstruction of anterior column by transforaminal approach with partial bone graft and Titaneum cage.
Take Home message –
To conclude, unstable thoracolumbar junctional fracture are known to cause neurological deficit though that is not the rule. Neurological deficit and structural instability dictates Surgical Intervention Classifying the grade of Instability and establishing level of neurological deficit is paramount. Pendulum is shifting towards all posterior spine surgery. Every fracture is unique and management is tailor made. Depending on Fracture pattern, stability, neurology and disruption of ligament complex will dictate the treatment protocol. Anterior versus posterior, short versus long fixation, open decompression versus indirect decompression have been issues. In today’s era, every treatment protocol is evidence based and result oriented. Issues of anterior surgery are well described, morbidity of approach, risk to major vascular structures and organs, need definite consideration. We have given algorithm depending on the literature and their clinical experience over years of managing thoracolumbar fractures.
References
1. Rajasekaran S, Thoracolumbar burst fractures without neurological deficit: the role for conservative treatment, Eur Spine J. 2010 Mar;19 Suppl 1:S40-7.
2. Dennis F. The three column spine and its signifi cance in the classifi cation of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 8(8):817-831.
3. Tator CH, Koyanagi I (1997) Vascular mechanisms in the pathophysiology
of human spinal cord injury. J Neurosurg 86:483– 492
4. Steven C. Kirshblum et al, International standards for neurological classification of spinal cord injury (Revised 2011) J Spinal Cord Med. 2011 Nov; 34(6): 535–546.
5. Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 1969;7(3):179–192
6. American Spinal Injury Association: International Standards for Neurological Classification of Spinal Cord Injury, revised 2000; Atlanta, GA, Reprinted 2008.
7. Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Joint Surg Br. 1949; 31(3):376-395.
8. Panjabi MM, Thibodieau LL, Crisco JJ, White AA. What constitutes spinal instability? Clin Neurosurg. 1988; (34):313-319
9. Bohler L. Die techniek de knochenbruchbehandlung imgrieden und im kriege. Verlag von Wilhelm Maudrich 1930 (in German).
10. Joon Y. Lee et al, Thoracolumbar injury classification and severity score: a new paradigm for the treatment of thoracolumbar spine trauma, J Orthop Sci (2005)
11. McCormack, Thomas MD; Karaikovic, Eldin MD; Gaines, Robert W. MD
Spine:The Load Sharing Classification of Spine Fractures, SPINE vol9, pp1741-1744, J.B Lippincott
12. Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine 1994;3: 184-201.
13. Alexander R. Vaccaro et al, AOSpineThoracolumbar Spine Injury Classification System, SPINE Volume 38, Number 23, pp 2028-2037 Spine 2013, Lippincott Williams & Wilkins
14. Fan KF, Tu YK, Hsu RW et al (1997) The high fixation failure rate of short segment pedicle instrumentation for unstable thoracolumbar burst fractures. Orthop Trans 21:267
15.Celibi L, Muratli HH, Dogan O et al (2004) The efficacy of nonoperative treatment of burst fractures of the thoracolumbar vertebrae. Acta Orthop Traumatol Turc 38(1):16–22
16. Shen WJ, Liu TJ, Shen YS (2001) Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine 26:1338–1345
17. Lu J, Ashwell KW, Waite P (2000) Advances in secondary spinal cord injury: role of apoptosis. Spine 25:1859–1866
18. Bohlman HH, Freehafer A, Dejak J. The results of treatment of acute injuries of the upper thoracic spine with paralysis. J Bone Joint Surg Am 1985;67A:360–369
19. Bellabarba C, Fisher C, Chapman JR, Dettori JR, Norvell DC. Does early fracture fixation of thoracolumbar spine fractures decrease morbidity or mortality? Spine (Phila Pa 1976). 2010 Apr 20;35(9 Suppl):S138-45.
20. Wu H, Fu C, Yu W, Wang J. The options of the three different surgical approaches for the treatment of Denis type A and B thoracolumbar burst fracture. Eur J Orthop Surg Traumatol. 2014 Jan;24(1):29-35.
21. Zahra B, Jodoin A, Maurais G, Parent S, Mac-Thiong JM. Treatment of thoracolumbar burst fractures by means of anterior fusion and cage. J Spinal Disord Tech. 2012 Feb;25(1):30-7.
22. Schnee CL, Ansell LV. Selection criteria and outcome of operative approaches for thoracolumbar burst fractures with and without neurological deficit. J Neurosurg. 1997 Jan;86(1):48-55
23. M. Payer. Unstable burst fractures of the thoraco-lumbar junction: treatment by posterior bisegmental correction/fixation and staged anterior corpectomy and titanium cage implantation Acta Neurochir (Wien) (2006) 148: 299
24. Kaya RA, Aydin Y. Modified transpedicular approach for the surgical treatment of severe thoracolumbar or lumbar burst fractures. Spine J. 2004 Mar-Apr;4(2):208-17
25. Altay M, Ozkurt B, Aktekin CN, Ozturk AM, Dogan O, Tabak AY. Treatment of unstable thoracolumbar junction burst fractures with short- or long-segment posterior fixation in magerl type a fractures. Eur Spine J. 2007;16:1145–1155
26. Limb D, Shaw DL, Dickson RA. Neurological injury in thoracolumbar burst fractures. J Bone Joint Surg Br. 1995; 77(5):774–777
27. Wilcox R, Boerger T, Allen D, et al. A dynamic study of thoracolumbar burst fractures. J Bone Joint Surg Am. 2003; 85(11):2184–2189
28. Boerger TO, Limb D, Dickson RA. Does ‘canal clearance’ affect neurological outcome after thoracolumbar burst fractures?J Bone Joint Surg Br. 2000; 82(5):629–635.
| How to Cite this Article: Khurjekar K, Kulkarni H, Kardile M. Treatment Algorithm for Unstable Burst Fractures . International Journal of Spine Sep-Dec 2016;1(2):27-32. |