Management of Pathological vertebral collapse in elderly
Volume 1 | Issue 2 | Sep – Dec 2016 | Page 22-26 | Rajesh Parasnis, Alpesh Thumbadiya, Sachin Pathak, Shantanu Patil
Authors : Rajesh Parasnis [1], Alpesh Thumbadiya [1], Sachin Pathak [1], Shantanu Patil [1]
[1] Oyster and pearl hospital, Pune
[2] Jehangir Hospital, Pune
[3] SRM Medical College, SRM University, Kattankulathur, Tamil Nadu 603203
Address of Correspondence
Dr. Rajesh Parasnis
Department of Spine Surgery, Oyster and pearl hospital, India.
Email : rajeshparasnis@rediffmail.com
Abstract
Pathological vertebral fractures can be due to various reasons and management plans will differ as per the diagnosis. We present our series of patient with pathological fractures along with a management algorithm
Material and Methods: All patients aged more than 60 years presenting with intractable back pain with or without neurological deficit were screened. Of the 532 patients, 274 osteoporotic insufficiency fractures were identified by DEXA scan and excluded from the analysis. 258 patients with vertebral collapse caused by infection or neoplastic conditions were included in study.
Results: 212 patients (82.2%) had a single vertebral lesion followed by 34 (13.2%) at 2 levels and 12 (4.7%) with multiple vertebral levels involved. 161 cases (62.9%) had an infective pathology while the remaining 97 (37.9%) had a neoplastic cause. Needle biopsy was positive in 218 (84.49% ) cases. Repeat biopsy was required in 39 cases where Fine Needle Aspiration Cytology (FNAC) was inconclusive. There were 130 tubercular lesion, 7 atypical tuberculosis, 5 MDR tuberculosis, 13 pyogenic, 2 fungal, 4 hydatid cyst, 24 malignant lesions and 73 metastasis. 60 patients (58 TB spine and 2 pyogenic infection) were managed without surgery and the remainder 197 patients underwent surgical intervention
Conclusion: Pathological fractures can be due to varied etiology and although tuberculosis formed major cohort in our series, neoplastic lesion had to be suspected and tissue biopsy is essential to reach correct diagnosis and management plan
Keywords: Thoracolumbar fractures, pathological fractures, biopsy.
Introduction
Atraumatic vertebral collapse is a common clinical problem, especially in elderly population (1). It includes fractures because of osteoporosis or any other pathological cause. Pathological vertebral fracture in elderly occurs due to infective or neoplastic condition. Spinal column affection by neoplastic lesions include primary (benign or malignant ) or secondary metastasis. 50 to 85% of patients with cancer experience skeletal metastasis, most commonly in the spine (2). Infection of spine occurs due to tuberculosis, atypical tuberculosis, pyogenic, fungal and parasitic infestation (e.g.hydatid cyst). Tuberculosis is most common among them and a major health problem in developing countries. In elderly population because of comorbidity and lower immunity, spinal affection by tuberculosis is high.
The spine has a load-bearing and a neuro-protective function, Any failure of its structural integrity as a result of metastatic or infective vertebral involvement often brings about severe pain and/or paralysis. These symptoms impair the ambulatory ability of the patients and worsen their quality of life. One of the main causes of severe pain or paralysis is pathologic vertebral body collapse caused by an osteolytic lesion. Therefore, prevention and treatment of collapse is a key factor in maintaining the patients’ ambulatory ability especially in morbid elderly population (3,4,5,6). Early diagnosis of such conditions is very important to start with proper treatment.
Diagnosis of pathological vertebral collapse in aged population is usually missed or delayed. Elderly patients presenting with backache and vertebral collapse are a challenge for diagnosis as well as for management. Correct diagnosis may require all blood invastigations and imaging modalities including plain X-rays, ultrasonography (USG), computed tomography (CT), radionuclide bone scan, magnetic resonance imaging (MRI) and PET scan. For conclusive diagnosis one needs to identify the causative organism and know histopathology of the lesion by biopsy. One may need to repeat the biopsy if required before starting any treatment. It is mandatory to do a culture and test the sensitivity to rule out drug resistance in case of spinal tuberculosis. Management depends on multiple factors and requires multidisciplinary approach.
While many studies have investigated osteoporotic vertebral collapse in the elderly, not many have reported on other pathological fractures. We present our series of such patients and propose a treatment and management algorithm.
Methods and Materials
All patients aged more than 60 years presenting with intractable back pain with or without neurological deficit were identified from a data base spanning seven and half years (May 2008 to Nov 2015 ) at a tertiary care hospital. Of the 532 patients, 274 osteoporotic insufficiency fractures were identified by DEXA scan and excluded from the analysis. 258 patients with vertebral collapse caused by infection or neoplastic conditions were included in study. The patients were classified according to age, gender, pathology, levels affected, region involved, neurological deficit, type of biopsy and management protocol. Base line haematological tests included haemogram, liver function test (LFT), renal function test (RFT), CRP, ESR and serum electrophoresis studies. Radiological studies included Xrays of the affected region ( anteroposterior & lateral views ) and MRI were done in all cases. CT scan, Bone scan, PET scan and Bone marrow examination were done in indicated cases. Tissue diagnosis was done by biopsy in all cases for histopathology and/or culture sensitivity. Management protocol was decided according to the pathology and severity of the lesions. All patients were followed up at regular intervals 3 months, 6 months, 12 months and yearly follow up after that.
Results
The cohort included 258 patients (Male 156: Female 102) aged between 60 and 82 years age (mean age 63.4 years). 212 patients (82.2%) had a single vertebral lesion followed by 34 (13.2%) at 2 levels and 12 (4.7%) with multiple vertebral levels involved. 161 cases (62.9%) had an infective pathology while the remaining 97 (37.9%) had a neoplastic cause. Out of 258 patients mean aged 63.4 years ( 60-82 years ), we found 156 male and 102 female patients. Level of involvement was found to be single, double and multiple in 212 (82.17%), 34 (13.17%) and 12 (4.65%) cases respectively. Infective pathology was found in 161(62.89%) and neoplastic cause was found in 97(37.89%) cases. Distribution of pathology and level affected are detailed in Table 1.
Out of 258, 234 patients presented with intractable pain[predominant back pain in 198 (76.74%) and predominant extremity pain in 62 (24.03%) patients ] of mean duration8.2 weeks ( 1- 32weeks). 68 (26.35%) patients presented with neuro deficit( Frankel grade B in 3, C in 14 and D in 51 ). Constitutional symptoms were present in 38 (14.72) patients. Spinal deformity was present in 21 cases.
Biopsy: Diagnosis of pathological vertebral fracture in elderly age group is usually delayed but sometimes it may be wrongly diagnosed or even missed. Tissue diagnosis is mandatory in all cases. Needle biopsy using Jamshidi needle was done in all suspicious vertebral pathology. Biopsy material was sent for gram stain, Ziehl-Nielson stain, Pus culture and sensitivity, and histopathological examination. Acid fast bacteria culture was advised in relevant cases ( not responding to treatment and MDR Tb ). Gene expert study ( PCR ) for tuberculosis was done in last 2 years only. Needle biopsy was positive in 218 ( 84.49% ) cases. Repeat biopsy was required in 39 cases where Fine Needle Aspiration Cytology (FNAC) was inconclusive. Core biopsy was done in all these 39 cases using large bore Jamshidi needle and it showed malignancy in 19 cases and tuberculosis in 20 cases. In 11patients who had an unbiopsied vertebral lesion initially as primary lesion was confirmed, and not responding to chemotherapy or radiotherapy, a subsequent vertebral biopsy was done. 5 of these patients were diagnosed to have a tuberculous lesion. 27 vertebral collapse initially thought to be osteoporotic on radiological imaging ( MRI and DEXA ) but not responding to osteoporotic treatment were reevaluated by biopsy and turned out to be Koch’s spine in 21 cases and neoplastic in 6 cases. 17 patients who were put on AKT for Koch’s spine but not responding were reevaluated by biopsy and report turned out to be malignant lesion.
Management
60 patients (58 TB spine and 2 pyogenic infection) were managed without surgery and the remainder 197 patients underwent surgical intervention. Non surgical management comprised of bed rest, analgesics, bracing, anti microbial regimen according to pathogen in case of infective lesions.
The 58 patients of tubercular spondylitis were treated by ATT, 4 drug regimen ( Rifampicin, Isoniazide, Ethambutol, Pyrazinamide ) for 3 months, 3 drugs for 3 months, 2 drugs for 3 months. In 2 cases of pyogenic osteomyelitis culture sensitivity specific antibiotics were given intravenously for 2-3 weeks followed by orally for 6 weeks. CBC, CRP, ESR, LFT and RFT were done at regular interval to modify the dosage in all these old age patients.
In MDR cases second line drug therapy was administered and monitored by the Infectious disease specialist.
101 infective lesions were managed surgically ( 92 primary and 9 revision ).
53 patients of spinal tuberculosis were operated by posterior decompression and fixation. 28 patients underwent surgery by posterolateral extrapleural approach and anteroposterior reconstruction. 13 patients were operated by anterior approach for decompression and reconstruction. 7 patients required a combined surgery and reconstruction by anterior and posterior approaches.
All 97 neoplastic vertebral lesions required surgical intervention. Out of 24 primary malignant lesions 3 (out of 7) solitary plasmacytoma were removed enblock, rest all 21 cases were managed by intralesional removal of tumor mass. Pre operative embolisation was done in all vascular tumors ( Solitar plasmacytoma and spindle cell sarcoma ). 1 multiple myeloma and 2 implant related complications required revision surgery.
Out of 73 metastatic vertebral lesions, Vertebroplasty was done in 29 patients, kyphoplasty was done in 6 cases and surgery was done in 38 cases. En block removal was done in 4 patients while in rest 34 cases intralesional removal of tumor was done. Pre operative embolisation was done in all 38 operated cases. 7 cervical and 9 thoracolumbar lesions were operated by anterior approach, 13 thoracolumbar and lumbar lesions were operated by posterior approach, while 9 cases of thoracolumbar and lumbar lesions were dealt by combination of both anterior as well as posterior approach. All 38 operated cases of vertebral metastases were stabilized by at least 2 levels above and 2 levels below with cementation of involved vertebra in posterior approach and anterior reconstruction using cage with autograft.
Chemotherapy and/or radiotherapy was administered according to neoplastic pathology. Post operatively all malignant cases were put on bisphosphonate therapy.
Complications: 4 out of 197 surgically operated elderly morbid patients died in the perioperative period.
Neurological and / or functional improvement was seen in 185 operated cases. Frankel grade B 3 patients improved to grade C in 1 and grade d in 2 cases. Frankel grade c 14 cases showed no improvement in 3 cases, 9 improved to grade D and 2 improved to grade E. Out of 51 Frankel grade D, 4 patients didn’t show much improvement but 37 fully recovered. Operated Koch’s spine all patients showed neurological improvement.
Mean survival time in primary malignancy cases was 36.2 months, while in metastatic cases it was 14.3 months. 7 patients developed recurrence at same level after mean time of 9 months, out of those 2 patients developed paraplegia.
Discussion
Atraumatic vertebral collapse is a common clinical problem, especially in elderly population (1). Osteoporotic vertebral fracture is the major cause in such elderly population. The prevalence of osteoporotic vertebral fractures varied from about 3% in the age group below 60 to about 19% in the 70+ group in women, and from 7.5% to about 20% in men, with an overall prevalence of 11.8% in women and 13.8% in men (7). Among other causes of pathological collapse in the elderly, infective lesions are also common with neoplastic lesions being on the higher side. A fairly high index of suspicion is necessary when dealing with vertebral collapses in the elderly population.
Infection of spine is still a mojor health issue in developing countries. Poor hygiene, poverty, unawareness, poor ventilation along with that other co-morbidities make elderly individual more prone for the infection especially tubercular in developing countries.
With ageing bony trabeculae becomes weak and osteoporotic vertebral collapse become more prevalent. Because the spine has a load-bearing and a nerve-protecting function, failure of its structural integrity as a result of pathological vertebral involvement often brings about severe pain and/or paralysis. These symptoms impair the ambulatory ability of the patients and worsen their quality of life. One of the main causes of severe pain or paralysis is pathologic vertebral body collapse caused by an osteolytic lesion. Therefore, prevention and treatment of collapse is a key factor in maintaining the patients’ ambulatory ability especially in morbid elderly population (3,4,5,6). So early diagnosis of such conditions is very important to start with proper treatment.
Tan DY et al., studied 58 vertebral collapse out of which he found 36 benign vertebral collapses (20 osteoporotic, 7 post-traumatic, 9 infective) and 22 malignant ones (20 metastatic carcinoma, 2 multiple myeloma). In our study we found Infective pathology in 161 (62.89%) [ 13 pyogenic, 130 tubercular, 7 atypical tubercular, 5 MDR tubercular, 2 fungal, 4 hydatid cyst ] and neoplastic lesions in 97 (37.89%) [ 24 primary malignant ( 13 multiple myeloma, 7 solitary plasmacyetoma, 3 lymphoma, 1 spindle cell sarcoma ) and 73 metastases ].The most frequent spinal metastases (60%) are from breast, lung, or prostate cancer (15).
Any elderly patient presenting with intractable back pain especially at night, weight loss and other constitutional symptoms without any history of trivial injury then think of pathological vertebral lesion. Any vertebral collapse detected on a radiograph must initially undergo MRI and routine blood investigations, followed by a DEXA scan to rule out osteoporosis. Even though DEXA scan is indicating osteoporosis it doesn’t always rule out infection or malignancy. In our study we found 27 patients with osteoporotic vertebral collapse, who didn’t respond to osteoporotic treatment and later on confirmed by biopsy as malignancy in 6 cases and infection in 21 cases.
Typical spinal tuberculosis affects the continuous vertebral levels and causes narrowing of the adjacent disc space and bone destruction (8). However, Atypical tuberculous spondylitis shows spondylitis without discitis, isolated central lesion in single vertebral body, non-contiguous skip vertebral body lesions, isolated posterior vertebral elements involvement and isolated intraspinal canal lesions. Atypical form of spinal tuberculosis is difficult to distinguish from malignancy, leading to misdiagnosis and inadequate treatment. Pyogenic and fungal spondylitis, sarcoidosis, metastasis and lymphoma are the close differential diagnosis for tuberculous spondylitis (10, 11).
Differentiating tuberculous spondylitis from these conditions is very important since the line of management completely differs and also early intervention helps in minimizing the residual spinal deformity and permanent neurological deficits (12). Tan DY et al. stated that features which pointed to malignant cause were hypointense marrow on T1-weighted images, marrow enhancement after intravenous contrast, greater than 50% marrow involvement and involvement of posterior elements. Of the vertebral collapses due to infection, 78% showed end-plate disruption(14). Image guided biopsy is very helpful for early diagnosis and prompt intervention if the clinical and imaging findings are not very helpful arriving diagnosis, especially with the atypical presentations (13).
Biopsy: Diagnosis of pathological vertebral fracture in elderly age group is usually delayed but sometimes it may be wrongly diagnosed or even missed. Tissue diagnosis is mandatory in all cases. Needle biopsy is the procedure of choice in definitive diagnosis of pathologic lesions of the spine (17). Needle biopsy is positive in 65% for lytic lesions, incisional biopsy is useful in 85% of blastic lesion while excisional biopsy is positive in >85% for posterior lesions and benign tumors. The percentage of positive results of biopsy are higher in metastases than primary tumors. The cystic and sclerotic vertebral tumors have less positive results. Transpedicular biopsy with Jamshidi needle has better success rate than FNAB in such lesions.
Once tissue diagnosis is done by biopsy then one should go ahead with other investigations such as CRP, ESR, Procalcitonin for infective pathology. For Neoplastic lesions one should do specific tumor markers and screening of whole body to rule out metastases elsewhere.
All Patients with spinal tuberculosis are started on antituberculosis treatment as Tuberculous spondylodiscitis is primary medical problem. Surgery reserved only for the patients with complications or potential complications (9). Only the patients who had lost neurological power to Frankel grade A,B,C,D or with sphincter involvement were advised surgery. 11 patients who did not show good response to ATT after 3 months were also operated. 17 patients who had progressive kyphosis and instability due to more than 2 vertebral level involvement were also advised surgery. Operative management gives satisfactory results in elderly patients with tuberculous spondylodiscitis (21). Single level involvement of spinal tuberculosis can be very well dealt by posterior approach only ( Transpedicular decompression, 2 level above and 2 level below fixation and shortening). The posterior approach provides adequate exposure for decompression and rigid fixation, providing satisfactory clinical and radiological outcomes (21).
2 level involvement requires pasterolateral extraplueral approach for decompression and reconstruction ( 3 or 4 level above and below ). In case of more than 2 levels are involved one should think of anterior or anterior and posterior approach for thorough decompression and stabilization of segment involved.
The pathological fractures due to neoplastic inlvolvement require a thorough check up to determine the general condition of the patient, staging and grading of the tumor, life expectancy , anticipated hospital and ICU stay etc. The indications for surgery for primary lesions are neurological deficit, instability, intratctable pain, radioresistant tumor and not sensitive to chemotherapy. The metastatic lesion may need surgery for severe pain, progressive neurogical deficit, instability affecting ambulatory ability or solitary metastases where in complete excision may be advocated.
The decision of surgery in malignant or metastatic lesion is taken only if the general condition allows the patient to recover without significant postoperative morbidity or ICU stay.
Vertebroplasty or kyphoplasty is the modality used in such inoperable painful collapse. Transpedicle body augmenter Vertebroplasty proved to be safe and effective in reducing pain andimproving functional status of patients with spinal tumor (18). Percutaneous Vertebroplasty (PVP) can be an effective treatment for metastatic spinal tumors in patients even with posterior wall deficiency (16).
Takayuki Yamashita stated that palliative surgery benefited half of the patients with metastatic spinal tumor, with a greater probability of benefit found in persons with a higher total revised Tokuhashi score (score 9–15) and/or primary cancers with longer survival times (19).
The modified Tokuhashi scoring system is used to decide the operability of the tumor.
The type of surgery and approach is decided depending upon primary or metastasis, extent of involvement of vertebra (Tomita classification) and expected morbidity of the surgery. The response of the tumor to radiotherapy and chemotherapy is also an important factor in management. David W. Polly et al concluded that there is a strong recommendation for posterior or posterolateral approach from T2 through T5. For the T6–L5 regions of the spine we recommend either anterior, posterior, or combined anterior and posterior surgery depending on the clinical presentation, surgeon and patient preference (20).
Hormonal treatment and immunotherapy may play an important role in certain tumors like Ca breast, ovary. In some inoperable tumors management to control pain is very important.
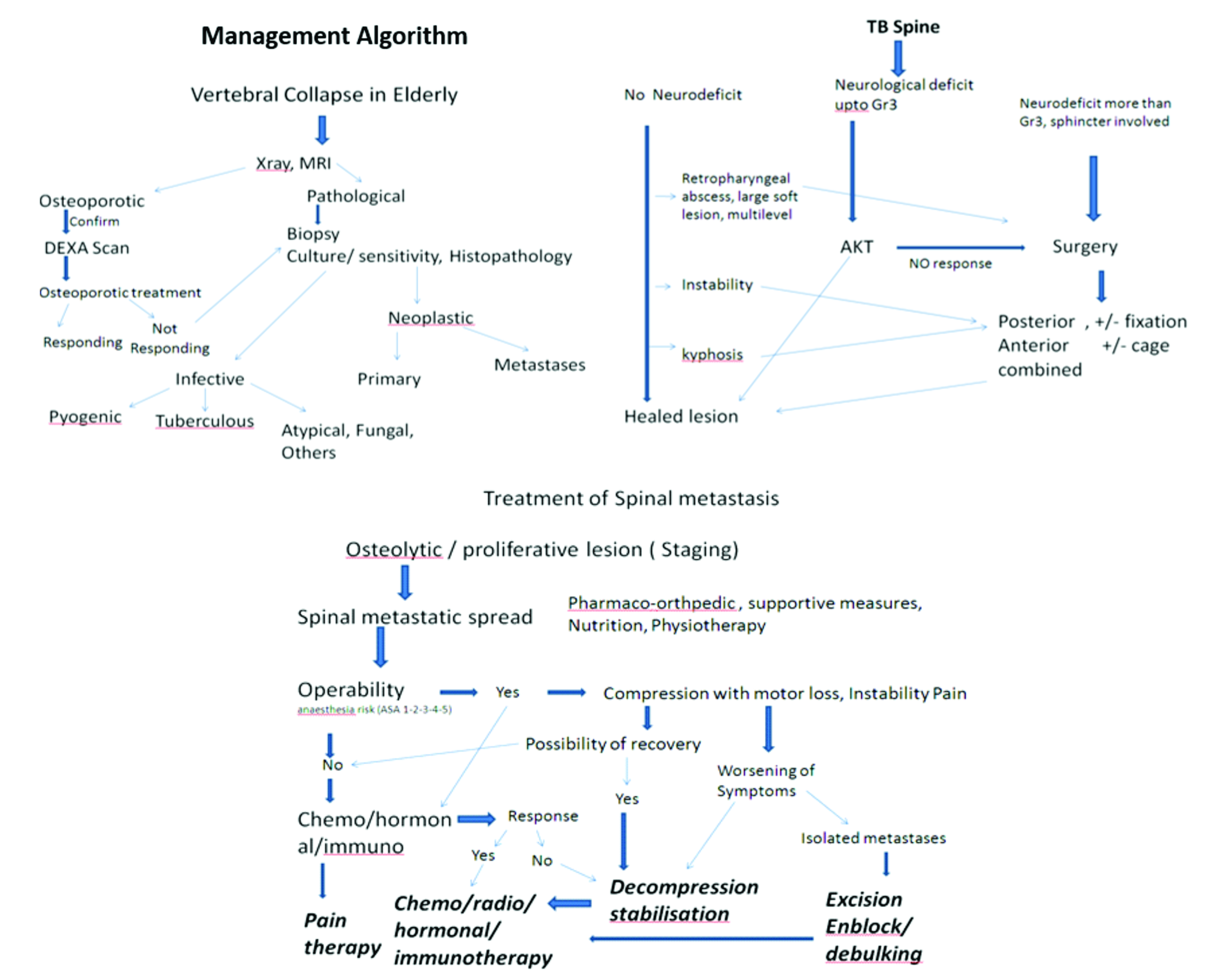
The pathological fractures in elderly can be managed by the following algorithms.
References
1. Cicala D, Briganti F, Casale L, et al. Atraumatic vertebral compression fractures: differential diagnosis between benignosteoporotic and malignant fractures by MRI. MusculoskeletSurg 2013;97(Suppl. 2):169–79.
2. Asdourian PL. Metastatic disease of the spine. In: Bridwell KH, DeWald RL, eds. The Textbook of Spinal Surgery. Philadelphia, JB Lippincott, 1991:1187-242. [Context Link]
3. Cybulski GR. Method of surgical stabilization for metastatic disease of the spine. Neurosurgery 1989;25:240-52. Buy Now Bibliographic Links [Context Link]
4. Hammerberg KW. Surgical treatment of metastatic spine disease. Spine 1992;17:1148-53. [Context Link]
5. Sundaresan N, Galicich JH, Lane JM. Harrington rod stabilization for pathological fractures of the spine. J Neurosurg 1984;60:282-6.Bibliographic Links [Context Link]
6. Matsubayashi T, Koga H, Nishiyama Y, et al. The reparative process of metastatic bone lesions after radiotherapy. Japan J ClinOncol 1981;11(Suppl):253. [Context Link]
7. Svanhild Waterloo, Luai A Ahmed et al. Prevalence of vertebral fractures in women and men in the population-based Tromsø Study. BMC Musculoskeletal Disorders 2012, 13:3
8. Naim-Ur-Rahman, El-Bakry A, Jamjoom A, et al. Atypical forms of spinal tuberculosis: case report and review of the literature. Surg Neurol. 1999;51(6):602- 07.
9. Rasouli MR, Mirkoohi M, Vaccaro AR, Yarandi KK, Rahimi-Movaghar V. Spinal Tuberculosis: Diagnosis and Management. Asian Spine J. 2012;6(4):294–308.
10. Jung NY, Jee WH, Ha KY, Park CK, Byun JY. Discrimination of tuberculous spondylitis from pyogenic spondylitis on MRI. AJR Am J Roentgenol. 2004;182(6):1405-10.
11. Khattry N, Thulkar S, Das A, Alan Khan S, Bakhshi S. Spinal tuberculosis mimicking malignancy: Atypical imaging features. Indian J Paediatr. 2007;74(3):297-8. PMID: 17401273.
12. Moore SL, Rafii M. Imaging of musculoskeletal and spinal tuberculosis. RadiolClin North Am. 2001;39(2):329-42.
13. Momjian R, George M. Atypical Imaging Features of Tuberculous Spondylitis: Case Report with Literature Review. J Radiol Case Rep. 2014;8(11):1–14.
14. Tan DY , Tsou IY , Chee TS. Differentiation of malignant vertebral collapse from osteoporotic and other benign causes using magnetic resonance imaging. Annals of the Academy of Medicine, Singapore [2002, 31(1):8-14]
15. Max Aebi. Spinal metastasis in the elderly .Eur Spine J (2003) 12 (Suppl. 2) : S202–S213
16. Hongpu Sun et al Safety of percutaneous vertebroplasty for the treatment of metastatic spinal tumors in patients with posterior wall defects. Eur Spine J (2015) 24:1768–1777
17. J. Tehranzadeh, C. Tao & C. A. Browning (2007) Percutaneous Needle Biopsy of the Spine, Acta Radiologica, 48:8, 860-868.
18. Anna F-Y. Li, Kung-Chia Li, Fang-Yuan Chang and Ching-Hsiang Hsieh. Preliminary Report of Transpedicle Body Augmenter Vertebroplasty in Painful Vertebral Tumors. SPINE Volume 31, Number 21, pp E805–E812 ©2006.
19. Takayuki Yamashita, Yoichi Aota et al Changes in Physical Function After Palliative Surgery for Metastatic Spinal Tumor Association of the Revised Tokuhashi Score With Neurologic Recovery. SPINE Volume 33, Number 21, pp 2341–2346 ©2008
20. David W. Polly, Jr, Dean Chou et al. An Analysis of Decision Making and Treatment in Thoracolumbar Metastases. SPINE Volume 34, Number 22S, pp S118–S127 ©2009.
21. Manish Kothari, Kunal Shah, Agnivesh Tikoo, Abhay Nene. Short to Mid-Term Term Surgical Outcome Study with Posterior Only Approach on Tuberculous Spondylodiscitis in an Elderly Population. Asian Spine J 2016;10(2):258-266.
| How to Cite this Article: Parasnis R, Thumbadiya A, Pathak S, Patil S. Management of Pathological vertebral collapse in elderly. International Journal of Spine Sep-Dec 2016;1(2):22-26. |
(Abstract) (Full Text HTML) (Download PDF)
Taking IJS Ahead
Volume 1 | Issue 2 | Sep – Dec 2016 | Page 1-2 | Ketan Khurjekar [1], Shailesh Hadgaonkar [1], Ashok Shyam [1,2]
Authors : Ketan Khurjekar [1], Shailesh Hadgaonkar [1], Ashok Shyam [1],[2]
[1] Sancheti Institute for Orthopaedics &Rehabilitation, Pune, India
[2] Indian Orthopaedic Research Group, Thane, India
Address of Correspondence
IJS Editorial Officie
A-203, Manthan Apts, Shreesh CHS, Hajuri Road, Thane [W]
Maharashtra, India.
Email: editor.ijspine@gmail.com
International Journal of Spine has made its mark from the release of first issue and in the second issue we have tried to make it better. As mentioned in the first editorial IJS has two main focus points, Research as well as Education. Currently most of the journals are focussed on research based articles and almost 90% of their publication is original articles. IJs is planned to take a different route where we wish to include equal amount of educational material in the journal.
Every issue of IJS is planned to contain a symposia on a specific topic. These symposia are solicited from leading spine surgeons in the field and are formatted in form of a review article which is easy to read. We encourage authors to include case based scenarios in the review which become much easier to relate to a clinician unlike articles full of statistics. The symposium are created in such a way that even small topics related to the scope of symposia are given adequate space and not become part of foot note. This approach will help general orthopaedic surgeons also who wish to refresh their knowledge and update themselves in the field of spine surgery. This will be especially useful to students who can get collection of articles on single topic written by best authors at one place. We will continue this trend of symposia in all future issue of IJS and invite suggestions from our readers for the topic of symposia. We also invite interested surgeons who wish to be symposium editors to contact the editorial office.
Short narrative reviews and literature updates also form the education element in IJS. One narrative review is published in this issue and from next issue the literature updates will start. It will include summary of most important articles and research that are published in other spine journals and are of practical importance to our readers. Original research articles and case reports will continue to be published in the journal but with strict review guidelines and will follow all ethical standards
From this issue we have started a new feature called ‘Interview’. IJS intends to interview the role models in field of spine surgery, especially people who inspire us to achieve excellence. The aim is to know them better and to understand their though process. We can learn many things from them even outside orthopaedics and this aspect comes out beautifully in the current interview of Dr S Rajasekaran. He was gracious enough to give us his precious time and share with us his knowledge and principles that he follows in his life. We believe this interview will inspire many and everyone will learn something valuable from it. The interview was almost two hours long and in this issue we could include only the part of the interview. The second part will be published in the forthcoming issue. We wish to continue this feature and will be interviewing many more stalwarts in the field of Spine surgery.
IJS is receiving more and more submissions each day and we wish to continue publishing good quality articles. We will appreciate any suggestions of comments, please write to us by email to editor.ijspine@gmail.com.
Dr. Ketan Khurjekar | Dr. Shailesh Hadgaonkar | Dr. Ashok Shyam
| How to Cite this Article: Khurjekar K, Hadgaonkar S, Shyam A. Taking IJS Ahead. International Journal of Spine Sep – Dec 2016;1(2):1-2. |
(Abstract) (Full Text HTML) (Download PDF)
Cervical Ossified Posterior Longitudinal Ligament
Volume 1 | Issue 2 | Sep – Dec 2016 | Page 49-51 | Kunal Shah, Manish Kothari, Abhay Nene
Authors : Kunal Shah [1], Manish Kothari [1], Abhay Nene [1]
[1] Department of Spine Surgery, Wockhardt Hospital and
Medical Research Centre Agripada, Dr Anand Rao Nair Road
Mumbai Central, Mumbai. India – 400008
Address of Correspondence
Dr. Abhay Nene
Department of Spine Surgery, Wockhardt Hospital and
Medical Research Centre Agripada, Dr Anand Rao Nair
Road,Mumbai Central, Mumbai. India – 400008
Email: abhaynene@yahoo.com
Abstract
Introduction
Cervical ossified posterior longitudinal
ligament is a common cause of myelopathy.
It is frequently encountered in busy spine
clinic with varied presentation; however
there are lots of controversies in this topic.
Etiopathogenesis and natural history is
unknown and progression is unpredictable.
Timing of surgery and type of approach is
also controversial and many factors should
be taken into account for surgical planning.
References
1) Yonenobu K. Is surgery indicated for asymptomatic or mildly
myelopathic patients with significant ossification of the posterior
longitudinal ligament? Spine (Phila Pa 1976). 2012 Mar
1;37(5):E315-7.
2) Wilson JR, Patel AA, Brodt ED, Dettori JR, Brodke DS, Fehlings MG.
Genetics and heritability of cervical spondylotic myelopathy and
ossification of the posterior longitudinal ligament: results of a
systematic review. Spine (Phila Pa 1976). 2013 Oct 15;38(22 Suppl
1):S123-46.
3) Chiba K , Yamamoto I , Hirabayashi H , et al. Multicenter study to
investigate postoperative progression of the posterior longitudinal
ligament in the cervical spine using a new computer-assisted
measurement . J Neurosurg Spine 2005 ; 3 : 17 – 23 .
4) Choi BW, Baek DH, Sheffler LC, Chang H. Analysis of progression of
cervical OPLL using computerized tomography: typical sign of
maturation of OPLL mass. J Neurosurg Spine. 2015 Jul 17:1-5.
5) Matsunaga S , Sakou T , Hayashi K , et al. Trauma-induced
myelopathy in patients with ossifi cation of the posterior longitudinal
ligament . J Neurosurg 2002 ; 97 : S172 – 5 .
6) Matsunaga S , Kukita M , Hayashi K , et al. Pathogenesis of
myelopathy in patients with ossifi cation of the posterior longitudinal
ligament . J Neurosurg 2002 ; 96 : S168 – 72 .
7) Matsunaga S, Nakamura K, Seichi A, Yokoyama T, Toh S, Ichimura S,
Satomi K, Endo K, Yamamoto K, Kato Y, Ito T, Tokuhashi Y, Uchida K,
Baba H, Kawahara N, Tomita K, Matsuyama Y, Ishiguro N, Iwasaki M,
Yoshikawa H, Yonenobu K, Kawakami M, Yoshida M, Inoue S, Tani T,
Kaneko K, Taguchi T, Imakiire T, Komiya S. Radiographic predictors
for the development of myelopathy in patients with ossification of the
posterior longitudinal ligament: a multicenter cohort study. Spine
(Phila Pa 1976). 2008 Nov 15;33(24):2648-50.
8) Rhee JM, Shamji MF, Erwin WM, Bransford RJ, Yoon ST, Smith JS,
Kim HJ, Ely CG, Dettori JR, Patel AA, Kalsi-Ryan S. Nonoperative
management of cervical myelopathy: a systematic review. Spine
(Phila Pa 1976). 2013 Oct 15;38(22 Suppl 1):S55-67.
9) Yoon ST, Raich A, Hashimoto RE, Riew KD, Shaffrey CI, Rhee JM,
Tetreault LA, Skelly AC, Fehlings MG. Predictive factors affecting
outcome after cervical laminoplasty. Spine (Phila Pa 1976). 2013 Oct
15;38(22 Suppl 1):S232-52.
10) Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K,
Yoshikawa H. Surgical strategy for cervical myelopathy due to
ossification of the posterior longitudinal ligament: Part 2: Advantages
of anterior decompression and fusion over laminoplasty. Spine (Phila
Pa 1976). 2007 Mar 15;32(6):654-60.
11) Suda K , Abumi K , Ito M , et al. Local kyphosis reduces outcomes of
expansive open-door laminoplasty for cervical spondylotic
myelopathy . Spine 2003 ; 28 : 1258 – 62 .
12) Sakai K, Okawa A, Takahashi M, Arai Y, Kawabata S, Enomoto M,
Kato T, Hirai T, Shinomiya K. Five-year follow-up evaluation of
surgical treatment for cervical myelopathy caused by ossification of
the posterior longitudinal ligament: a prospective comparative study
of anterior decompression and fusion with floating method versus
laminoplasty. Spine (Phila Pa 1976). 2012 Mar 1;37(5):367-76.
13) Katsumi K, Izumi T, Ito T, Hirano T, Watanabe K, Ohashi M. Posterior
instrumented fusion suppresses the progression of ossification of the
posterior longitudinal ligament: a comparison of laminoplasty with and
without instrumented fusion by three-dimensional analysis. Eur Spine
J. 2015 Nov 19. [Epub ahead of print]
14) Wei-bing X , Wun-Jer S , Gang L , et al. Reconstructive techniques
study after anterior decompression of multilevel cervical spondylotic
myelopathy . J Spinal Disord Tech 2009 ; 22 : 511 – 5 .
15) Yamaura I, Kurosa Y, Matuoka T, et al. Anterior floating method for
cervical myelopathy caused by ossification of the posterior
longitudinal ligament. Clin Orthop 1999;359:27–34.
| How to Cite this Article: Shah K , Kothari M , Nene A. Cervical Ossified Posterior Longitudinal Ligament. International Journal of Spine Sep-Dec 2016;1(2): 49-51. |
(Abstract) (Full Text HTML) (Download PDF)
An epidemiological study from a tertiary care hospital in Asian subcontinent on Traumatic cervical injuries: How is the injury pattern and what are the implications?
Volume 1 | Issue 2 | Sep – Dec 2016 | Page 44-48 | Dhiraj Vithal Sonawane, Ganesh Yeotiwad, Ajay Chandanwale, Swapnil Keny, Abhijeet Salunke, Ambarish Mathesul, Eknath Pawar
Authors : Dhiraj Vithal Sonawane [1], Ganesh Yeotiwad [1], Ajay Chandanwale [3], Swapnil Keny [1], Abhijeet Salunke [4], Ambarish Mathesul [3], Eknath Pawar [2]
[1] Department of Orthopaedics, Grant Medical college, & Gokuldas Tejpal Hospital, Mumbai
[2] Department Of Orthopaedics, Grant medical college, Mumbai.
[3] Sasoon Hospital & BJMC, Pune
[4] Gujarat Cancer Research Institute
Address of Correspondence
Dr. Dhiraj V. Sonawane
Grant Medical college, & Gokuldas
Tejpal Hospital, Mumbai
Email: dvsortho@gmail.com
Abstract
Objective: The aim of the current study was to document the demographic pattern, mode of injury, level of cervical spine injury in patients so that it can be extrapolated for formulating guidelines in developing nations for proper management of this life threatening injury.
Methods: This study comprised of 275 patients of cervical spine injury admitted in a tertiary care centre from January 2006 to October 2015.
Results: The mean age was (3 to 95) and male to female ratio was 11.5: 1. Majority (30 %) of cases were of third and fourth decade. 60 % of patient fall from height as mechanism of injury. The urban to rural ratio of patients was 3:1 and 184 patients (67%) belonged to the rural areas. The most common mode of injury in the present study was fall from height, 166 cases (60%) of which most of them occurred while working and fall from tree. Dislocation at C 5-6 vertebral level was commonest and a C 5 vertebra was most commonly fractured. Incomplete cord injury of ASIA grade C scale was the commonest pattern seen in 156 cases. Head injury was commonest associated injury with cervical spine injury.
Conclusion: Identification of demographic data and mechanism of injury pattern helps to identify the preventable risk factors for controlling them. Proper education and training of paramedical staff in rural areas of initial aid and transportation of patients having spinal cord injuries can reduce the frequency and morbidity of spine injuries
Keywords: Cervical spine, Injury, Epidemiology, demographic study, Spinal cord, Mechanism of injury
References
1. David O`Brien. Immediate management of spinal injury In: Jones D.
Palmar (compiler) manual of neurosurgery. First edition, UK,
Churchill, Livingston. 1996; 696-708
2. George W. Wood II, Campbell’s Operative Orthopaedics, 11th ed., vol
1, Elsevier, Philadelphia; 1761-1849.
3. Sinha DK. Manual of Patna Model for the care of Spinal cord injury
patients. Patna: Sparsh. 2000; 9-13.
4. Roopsingh et al. Traumatic spinal cord injuries in Haryana: An
Epidemiological study.Indian Journal of Community Medicine Vol.
XXVIII, No.4, Oct.-Dec., 2003.
5. Gunby I. New focus on spinal cord injury.JAMA.1981;245:1201–1206.
6. Botterell EH, Jousse AT, Kraus AS et al.A model for the future care of
acute spinal cord injuries.Can J NeurolSci. 1975; 2:361-80 .
7. Kraus JF. Injury to the head and spinal cord: The epidemiological
relevance of the medical literature published from 1960 to 1978.J
Neurosurg. 1980; S: S3-10.
8. Burney R.E. et al. Incidence ,Characteristicsand Outcome of Spinal
Cord Injury at Trauma Centers in North America .Arch Surg. 1993;
128 (5):p.596-9.
9. Fife D.andJ.Kraus .Anatomic Location of Spinal Cord Injury:
Relationship to the cause of injury. Spine. 1986; 11 (1):p.2-5.
10. Riggins R.S.and J.F.Kraus. The Risk of Neurologic Damage with
Fractures to the Vertebrae.The Journal of Trauma. 1977; 17 (2): p.
126-133.
11. Miller T.R.,et al. Costs of Head and Neck Injury and a Benefit –Cost.
12. Allen B.L. et al. A Mechanistic Classification of Closed,Indirect
Fractures and Dislocation of the Lower Cervical Spine. 1982;
7(1):p.1-27.
13. Burke D.C., H.T.Burleyand G.H.Ungar. Data on Spinal Injuries –Part
1.Collection and Analysis of 352 Consecutive Admissions
.AustrN.Z.Surg. 1985; 55:p.3-12.
14. Torg J.S., et al. National Football Head and Neck Injury Registry:
Report on Cervical Quadriplegia .AM J Sports Med. 1979;
7 (2):p.127-32.
15. Annamalai K, Chinnathambi R. Spinal cord injuires -The challenges
and the achievements. Chennai: Dept.of Orthopaedic Surgery,
Govt. General Hospital,Chennai.1998; 1-50.
16. Karacan I, Koyuncu H, Pekel O, Sumbuloglu G, KirnapM, Dursum
H et al. Traumatic spinal cord injuries inTurkey: a nationwide
epidemiological study. Spina Cord. 2000; 38(11): 697-701.
17. Hu R, Mustard CA, Burns C. Epidemiology of incident spinal
fracture in a complete population.Spine.1996; 21:492-499.
18. Chacko V, Joseph B, Mohanty SP, Jacob T. Management of spinal
cord injury in a general hospital in rural India. Paraplegia.1996; 24:
330-5.
19. A psychological study of spinal cord injured patients involved in the
Madras Paraplegia ProjectO Somasundaram, S Balakrishnan, O S
Ravindran, T K Shanmugasundaram.
20. Shingu H, Ikata T, Katoh S, Akatsu T. Spinal cord injuries in Japan:
A natiowide epidemiological survey in 1990. Paraplegia 1994;
32(1): 3-8.
21. Lan C, Lai JS, Chang KH, Kan YC, Lein In. Traumatic spinal cord
injuries in the rural region of Taiwan: an epidemiological study in
Hualien Country, 1986-1990. Paraplegia 1993; 31(6): 398-403.
22. Dave PK, Jayaswal A, Kotwal PP. Spinal cord injuries -A clinicoepidemiological
study. Ind J Orthop 2002; 28: 39- 45.
23. Singh M et al. Spine injuries in a tertiary health care hospital in
Jammu: A Clinico – Epidemiological Study. The Internet Journal of
Neurosurgery.
24. Shrestha D, Garg M, Singh GK, Singh MP, Sharma Uk.Cervical
spine injuries in a teaching hospital of eastern region of Nepal; A
clinic-epidemiological study. J Nepal med Assoc 2007; 46(167):
107-111.
25. Hadley MN, Zabramski JM, Browner CM, et al. Pediatric spinal
trauma:review of 122 cases of spinal cord and vertebral column
injuries. J Neurosurg.1988;68:18–24.
26. Carreon LY, Glassman SD, Campbell MJ. Pediatric spinefractures:
a review of 137 hospital admissions. J Spinal DisordTech.2004;
17:477–482.
27. Parisini P, Di Silvestre M, Greggi T. Treatment of spinal fractures in
children and adolescents: long-term results in 44patients. Spine.
2004; 27:1989–1994. Thesleff T, 28)Niskakangas T, Luoto TM,
Öhman J, Ronkainen A. Fatal cervical spine injuries: a Finnish
nationwide register-based epidemiologic study on data from 1987
to 2010. Spine J. 2015 Dec 7. pii: S1529-9430(15)01761-1.
29. Fredø HL, Rizvi SAM, Lied B, Rønning P, Helseth E. The
epidemiology of traumatic cervical spine fractures: a prospective
population study from Norway.Scandinavian Journal of Trauma,
Resuscitation and Emergency Medicine. 2012;20:85.
30. Hasler RM, Exadaktylos AK, Bouamra O, Benneker LM, Clancy M,
Sieber R, Zimmermann H, Lecky F. Epidemiology and predictors of
cervical spine injury in adult major trauma patients: a multicenter
cohort study. J Trauma Acute Care Surg. 2012 Apr;72(4):975-81.
31. Rahimi-Movaghar V, Sayyah M, K, Akbari H, Khorramirouz R,
Rasouli M, R, Moradi-Lakeh M, Shokraneh F, Vaccaro A, R,
Epidemiology of Traumatic Spinal Cord Injury in Developing
Countries: A Systematic Review. Neuroepidemiology 2013;41:65-
85
32. Sidong Yang, Wenyuan Ding, Dalong Yang, Tixin Gu, Feng Zhang,
Di Zhang, Yapeng Sun, Lei Ma, Yanli Song.Epidemiology and Risk
Factors of Cervical Spine Injury during Heating Season in the
Patients with Cervical Trauma: A Cross-Sectional Study PLoS One.
2013; 8(11): e78358.
| How to Cite this Article: Sonawane D V, Yeotiwad G, Chandanwale A, Keny S, Salunke A, Mathesul A, Pawar E.An epidemiological study from a tertiary care hospital in Asian subcontinent on Traumatic cervical injuries: How is the injury pattern and what are the implications?. International Journal of Spine Sep-Dec 2016; 1(2): 44-48. |
(Abstract) (Full Text HTML) (Download PDF)
Paraplegic Rehabilitation in Asia A Thoracolumbar Injuries – Options and Recent Advances
Volume 1 | Issue 2 | Sep – Dec 2016 | Page 22-26 | Kalidutta Das, Ansari Md. Neshar
Authors : Kalidutta Das [1], Ansari Md. Neshar1 [1]
[1] Oyster and pearl hospital, Pune
[2] Jehangir Hospital, Pune
[3] SRM Medical College, SRM University, Kattankulathur, Tamil Nadu 603203
Address of Correspondence
Dr. Rajesh Parasnis
Department of Spine Surgery, Oyster and pearl hospital, India.
Email : rajeshparasnis@rediffmail.com
Abstract
Traumatic paraplegic is a devastating injury due to spinal cord injury. Motor and sensory impairments along with bowel and bladder dysfunction causes activity limitation and causes severe impact on participation in life. The nature and severity of activity limitations and participation restrictions are dependent on the severity and site of the lesion as well as the person’s social roles and contextual Factors. The rehabilitation is crucial to prevent complications such as pressure ulcers, to improve functions and to assist with community integration and economic independence. Rehabilitation helps in attaining a reasonable degree of independence in performance of daily skill and reduction of disability. Interdisciplinary approach is optimum with the team being led by a physiatrist and involving patient and his family, physiotherapist, occupational therapist, dietician, psychologist, speech therapist, social worker and other specialist consultants.
References
1. William McKinley, Katia Santos, Michelle Meade, Karen Brooke.J
Spinal Cord Med. 2007; 30(3): 215–224.
2. Catz A, Itzkovich M, Steinberg F, Philo O, Ring H, Ronen J, et al. The
Catz-Itzkovich, SCIM: a revised version of the Spinal Cord
Independence Measure. Disabil Rehabil. 2001;23:263–268.
3. Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT,
Craven BC, et al. The Spinal Cord Independence Measure (SCIM)
version III: reliability and
validity in a multi-center international study. Disabil Rehabil.
2007;29:1926–1933
4. Ditunno Jr JF, Ditunno PL, Scivoletto G, Patrick M, Dijkers M, Barbeau
H, et al. The Walking Index for Spinal Cord Injury (WISCI/WISCI II):
nature, metric properties, use and misuse. Spinal Cord.
2013;51:346–355.
5. Harvey LA, Anderson KD. The spinal cord independence measure. J
Physiother.
2015;61:99.
6 . Harvey L, Marino R. The Walking Index for Spinal Cord Injury. Aust J
Physiother.
2009;55:66.
7. Pannek, J., Bersch, U.L.F. & Moulin, P. ArgoSpine News J. (2007) 16:
26. doi:10.1007/BF03041125
8. Gijnther M, L~Chner-Ernst D, Kramer G, Sti~Hrer M (2001j:
Auswirkungen Des Aseptischen Intermitiierenden Katheterismus Auf
Die M,~Nnliche Harnrohre. Urologe B 41; 359-361
9 . Schuhch B, ~I’oehrer M, Kramer G Etal (2000): Botulinum-A Toxin For
Treating Detrusor Hyperreflexia In Spinal Cord Injured Patients: A
New Alternative To Anticholinero)C Drugs? J Urol 164; 692-697
10. Reitz A, St~Hrer M, Kramer G Ef Al (2oo4): European Experience Of
200 Cases Treated With Botulinum-A Toxin ;Njections Into The
Detrusor Muscle Due To Neurogenic Oetrusor Overactfvit~ Eur Urol
45; 510 515
11.http://www.elearnsci.org/module.aspx?id=128&category=Doctors&mo
dule=Bladder+management&lesson=Overview
12. Kemal Nas, Levent Yazmalar, Volkan Şah, Abdulkadir Aydın, Kadriye
Öneş, Rehabilitation of spinal cord injuries World J Orthop. 2015 Jan
18; 6(1): 8–16. Published online 2015 Jan 18. doi:
10.5312/wjo.v6.i1.8
13. Mehrholz J, Kugler J, Pohl M. Locomotor training for walking after
spinal cord injury. Spine (Phila Pa 1976) 2008; 33: E768-E777 [PMID:
18827681 DOI: 10.1097/BRS.0b013e3181849747]
14. TRIUMPH, Spinal Cord Injury Guidelines. Deep Vein Thrombosis
Guidelines In Spinal Cord Injury.
15. American Occupational Therapy Association Occupational therapy
practice framework: domain and process. Am J Occup Ther
2002;56(6):609–39
16. http://www.spinalcord.com/blog/the-latest-medical-breakthroughs-forspinal-
cord-injuries
| How to Cite this Article: Das K, Neshar A. Paraplegic Rehabilitation in Asia A Thoracolumbar Injuries – Options and Recent Advances. International Journal of Spine Sep-Dec 2016;1(2): 39-43. |
(Abstract) (Full Text HTML) (Download PDF)
Minimally Invasive Spine Surgery Options in Management of Thoracolumbar Fractures- Indications and Surgical Techniques
Volume 1 | Issue 2 | Sep – Dec 2016 | Page 22-26 | Arvind Kulkarni, Sameer Ruparel
Authors : Arvind Kulkarni [1], Sameer Ruparel [1]
[1] Oyster and pearl hospital, Pune
[2] Jehangir Hospital, Pune
[3] SRM Medical College, SRM University, Kattankulathur, Tamil Nadu 603203
Address of Correspondence
Dr. Rajesh Parasnis
Department of Spine Surgery, Oyster and pearl hospital, India.
Email : rajeshparasnis@rediffmail.com
Abstract
Study Design: Literature review and expert opinion
Objective: Thoracolumbar fractures account for 90% of spine fractures. The conventional surgical treatment consists of open exposure with spinal instrumentation and fusion. With the advent of minimally invasive techniques and their approach related advantages combined with their successful use in degenerative disorders, they are being increasingly used in treatment of thoracolumbar injuries. The objective of this review article is to discuss indications and surgical techniques for the same.
Materials and Methods: A review of current English literature complemented with experience of the senior author was amalgamated.
Results: Current indications and surgical techniques of minimally invasive surgery along with the experience of the author are summarized.
Conclusion: The basic biomechanical principles of treatment of thoracolumbar fractures remain the same, irrespective of the approach. The scope of MIS for treating these injuries is increasing to encompass more complicated fracture patterns.
Key words: spine trauma, thoracolumbar, minimally invasive, instrumentation.
Introduction
Thoracolumbar fractures account for approximately 90% of all spine fractures [1]. Most of these are concentrated between D11 and L2 due to its transition from the rigid, stable kyphotic thoracic spine to mobile, lordotic lumbar spine and thus susceptible to injury. These injuries can result in potentially devastating sequelae including paralysis, pain, deformity, and loss of function [2–5]. In addition to the physical consequences, the long-term effects of spinal injuries may also have a significant psychologic, economic, and social impact [6–9]. The treatment goals for patients with thoracolumbar injuries are to maintain or restore spinal alignment and stability, preserve neurologic function and mobilize the patient as soon as possible. The conventional surgical treatment consists of open exposure with spinal instrumentation and fusion. With the advent of minimally invasive spine surgical techniques and successful utilization for lumbar degenerative disorders, these are increasingly used for the treatment of thoracolumbar fractures. Standard midline posterior spinal approaches have shown to cause significant muscle morbidity resulting from iatrogenic muscle denervation (particularly with exposure lateral to the facet), increased intramuscular pressures, ischemia and revascularization injury [10–14]. All these effects can lead to paraspinal muscular atrophy, scarring, and decreased extensor strength and endurance [15–20]. This approach related morbidity has prompted many spine surgeons to assess the feasibility of minimally invasive spine surgery for the treatment of thoracolumbar fractures. The objective of this review article is to discuss indications and surgical techniques for the same.
Indications and Surgical Technique:
Treatment of thoracolumbar fractures is controversial due to the lack of a classification system which incorporates the mechanism of injury and morphology of the fracture, has good inter observer reliability, neurological status of the patient and the condition of soft tissues. Due to this, it is often difficult to form a definite treatment algorithm for these fractures. However, principles of stabilization and fusion still remain the same irrespective of it being a conventional open or minimally invasive surgery. We used the ASIA scoring system to grade the neurological status of the patient. The AO classification system is used to describe the morphology of the fracture and treatment decision regarding surgery was based the Thoracolumbar Injury Classification and Severity [TLICS] Scale. Patients with progressive neurological deterioration and unstable fractures are frequently operated upon. The use of minimally invasive surgery seems to be a blessing in poly trauma patients requiring stabilization in view of Damage Control Orthopaedics [DCO].
Patients brought to casualty with thoracolumbar fractures are managed according to ATLS protocols. After stabilization, they are thoroughly evaluated and investigated. Classification of fracture and grading of neurological deficit is done as per above mentioned systems. Decision regarding surgery varies from patient to patient, generally patients with TLICS >= 4 are operated. Whether to apply minimally invasive surgical [MIS] techniques to treat these is dependent on numerous factors. MIS techniques are skilful and evidently have a steep learning curve. The surgeon must be thoroughly acquainted with the anatomy of the vertebral structures and MIS equipments. Hospital dependent factors include the availability of microscopes for adequate visualization, trained staff, MIS instrumentation and fluoroscopy. Navigation and use of intraoperative neurophysiological monitoring are additional factors which improve safety of the patient. The most important patient dependent factor is the cost. The benefits of reduced blood loss, infection rates, better tolerance to postoperative pain and faster recovery must be balanced with the cost involved in MIS instrumentation and implants.
Goals of surgery with thoracolumbar fractures include adequate biomechanical stabilization of the fractured segment, decompression of the neural structures and fusion of instrumented vertebrae. These are achieved with conventional open surgeries using anterior/ posterior approaches. Above can be achieved with minimally invasive surgical techniques as follows:
1. Percutaneous pedicle screw fixation- Percutaneous pedicle screw fixation restores the posterior tension band and indirectly augments the anterior column. These can be used when anterior fixation is not feasible and can augment anterior fixation. It is an excellent fixation technique in unstable polytrauma patients for initial stabilization. Typical indications of using these alone include fractures in which anterior column restoration is not required involving posterior elements e.g., Chance fracture i.e. flexion-distraction injuries of the spine.
2. Anterior minimal access decompression and stabilization: Anterior minimally invasive decompression and stabilization can be used independently or augmented with posterior percutaneous pedicle screw fixation and is typically employed in burst fractures wherein reconstruction of anterior column seems to be necessary. Decompression, stabilization and fusion can all be achieved with this approach.
3. Vertebroplasty/Kyphoplasty: This can be combined with percutaneous pedicle screw fixation in cases of pincer, wedge or incomplete burst fractures in middle aged adults, though traditionally vertebropalsty is used for osteoporotic fractures. After indirect reduction with patient positioning, although the vertebral walls give the radiological impression of a good reduction with the pedicle screw construct, the middle part of the endplate cannot be reduced [21]. The adjacent nucleus pulposus may later herniate through the fractured endplate resulting in anterior vertebral column insufficiency, progressive collapse and finally failure [22]. Thus, augmentation with vertebroplasty/ kyphoplasty seems to have a beneficial effect to the discs adjacent to an A3/AO-type fracture, managed with pedicle screw fixation plus endplate restoration, since no significant degeneration occurs 12–18 months post-injury [23].
Often, obtaining adequate anterior column stabilization and fusion with percutaneous pedicle screws and vertebraplasty/kyphoplasty is not feasibile. In these cases anterior approach is mandatory, though in incomplete/complete burst fractures manual reduction and transpedicular body augmentation with titanium spacers combining short segment fixation has been reported to be successful[24,25].
The current uses of MIS techniques and DL injuries where application of MIS can be considered and applied can be summarized as follows: [Table 1 and 2 respectively] by Rampersaud et al [26]:
Case Illustrations:
1. A 68 year old lady sustained L1 compression fracture without neurological deficit due to fall [Fig 1]. Patient was treated conservatively for 4 months elsewhere. Patient had persistent pain even after 4 months when repeat x-rays and MRI [Fig 2] showed further collapse of the fractures vertebra and was advised surgery. Patient underwent fixation with percutaneous pedicle screw fixation and vertebroplasty of fractured vertebra [Fig 3].
2. An 89 year old gentleman sustained an L3 vertebral fracture which was treated with vertebroplasty [Fig 4]. Patient complained of pain which was persistent for 4 months post vertebroplasty. Flexion extension x-rays [Fig 5] showed pseudoarthrosis of vertebral fracture, which was then treated with percutaneous cement augmented pedicle screws and vertebroplasty [Fig 6]. Presently, patient is symptomatically better.
3. A 52 year old gentleman suffered chance fracture D3-4 [Fig 7] without neurological deficit which was treated conservatively. 8 months following treatment patient developed myelopathic symptoms with repeat MRI [Fig 8] showing aggravation of radiographic features. Patient was operated with percutaneous pedicle screw fixation D2—5 [Fig 9].
Open Vs MIS in treatment of thoracolumbar fractures:
With increasing use of percutaneous pedicle screw fixation in the treatment of thoracolumbar fractures, studies have been conducted comparing clinical and radiological outcomes with conventional open pedicle screw fixation.
Wild et al in a study of 21 patients of AO Type 3 thoracolumbar compression injuries and concluded that percutaneous pedicle screw instrumentation [PPSI] was associated with significantly less blood loss with no difference in clinical and radiological outcomes 5 years after implant removal. The authors however observed increased operative time with PPSI [27]. Wang et al [28] in their study of 38 patients with similar injuries found significant decreases in operative time also along with other clinical and radiological parameters. While these previous studies retrospectively analysed 2 patient cohorts, Jiang et al. [29] recently published the only prospective randomized control trial comparing PPSI to an open paraspinal approach for thoracolumbar burst fractures in patients without neurological deficits. The authors demonstrated significant decreases in blood loss associated with PPSI compared to the paraspinal approach (79 ml vs 145 ml, respectively), a shorter hospital stay (9.7 vs 10.8 days, respectively) and less pain postoperatively. After more than 3 years of follow-up of 61 patients, there were no differences in Oswestry Disability Index score or VAS score. The paraspinal muscle group was able to achieve and maintain sagittal correction better than those obtained by the PPSI group. The authors concluded that PPSI offers improvements over the paraspinal approach.
Thus, above studies suggest the use of percutaneous pedicle screw instrumentation does have advantages over the conventional open approach whenever feasible.
Another fracture morphology that can be efficiently treated with MIS approaches is patients having flexion- distraction injuries. On comparison of radiological variables with MIS and open approaches, Grossbachet al[30]found though a slight increase in kyphosis [though not statistically significant] in MIS group post operatively. Joseph et al in their study of 15 cases with flexion distraction injuries [31], found that the average kyphosis improved from 19.6° preoperatively to 5.73° postoperatively, a statistically significant difference, and that the degree of kyphosis had increased to 7.87° at last follow-up, an increase that was not statistically significant. The average time to last follow-up was 16.1 months. The authors suggest that thoracic flexion-distraction injury may be amenable to this single surgical approach in most cases.
Many authors have raised concerns about the rates of screw malposition, adjacent facet violation and degeneration with PPSI. Panagiotis Korovessis et al, [32] in their retrospective study of 36 patients, found that 10% screws were malpositioned on axial CT images, four percent with each with grade II and grade III malpositions. Patients with grade III malposition reported lower extremity discomfort without neurological deficit. Intraarticular adjacent segment facet violation by the pedicle screws was disclosed in axial CT images in eight (5.5 %) facet joints. Adjacent joint degeneration at the violated by screw facet was shown in 2 (5.5 %) patients, respectively, 1 year post-operation. Spontaneous inter-facet fusion within the instrumentation area at the 1 year f/up occurred in 10/36 (28 %) patients. On comparison of these statistics with conventional open approach, Chen et al [33] reported 24–100 % facet joint violation rates in open , while other studies reported 11–50 % violation rates for percutaneous procedures [34,35]. However, Panagiotis Korovessis et al, [32] reported much lower facet joint violation rates [5.5%].
PPSI along with vertebroplasty/kyphoplasty for the reconstruction of anterior column has shown good clinical and radiological outcomes. With 18 patients suffering from lumbar compression and burst fractures, Korovessis et al [32] found the mean blood loss and operative times to be 75 ml and 45 minutes respectively. Segmental kyphosis decreased from 16 to 2 degrees with no neurological complications. Though, Rahamimov et at [36] in a similar study found of 52 patients, reported 3 cases of PMMA emboli, and in half of the patients there was a cement leak into adjacent soft tissue either through the fracture or through segmental veins but no cases of extravasation into the spinal canal suggesting potential complications of this technique.
For thoracolumbar injuries with requiring more extensive anterior reconstruction and decompression, Kim et al [37] reported 85% fusion rates for stand alone procedures and 90% for combined procedures. They performed thoracoscopic decompression, reconstruction and instrumentation in 212 patients with AO type A, B and C fractures. However, 64% underwent standard open posterior stabilization. Three cases required conversion to open procedure. 90% patients maintained sagittal alignment at 1 year follow up.
Use of the transpsoas or lateral approach to the lumbar and thoracolumbar spine has been increasing over the last decade in the treatment of degenerative conditions [38, 39]. Smith et al. [40]used this approach in the treatment of 52 patients with AO Type B and C fractures. Expandable titanium cages were used for anterior column support supplemented with anterolateral fixation or pedicle screws or combination of thereof. Mean operative time and blood loss were 127 minutes and 300 ml respectively with complication rates reported to be 15%.
Thus, majority of thoracolumbar fractures are amenable to minimally invasive techniques and these are increasing used successfully for their treatment as evident in above mentioned studies.
References
1. DeWald RL. Burst fractures of the thoracic and lumbar spine. ClinOrthopRelat Res.1984; (189): 150–161.
2. Gertzbein SD. Scoliosis Research Society: Multi center spine fracture study. Spine 1992; 17: 528–40.
3. Levine A, McAfee P, Anderson P. Evaluation and emergent treatment of patients with thoracolumbar trauma. Instr Course Lect 1995; 44: 33–45.
4. McCormack B, MacMillan M, Fessler R. Management of thoracic, lumbar and sacral injuries. In: Tindall G, Cooper P, Barrow D, Eds. The Practice of Neurosurgery. Baltimore: Williams & Wilkins, 1996.
5. Meldon S, Moettus L. Thoracolumbar spine fractures: clinical presentation and the effect of altered sensorium and major injury. J Trauma 1995; 39: 1110–4.
6. Bosch A, Stauffer E, Nichel V. Incomplete traumatic quadriplegia: a ten year review. JAMA 1971; 216: 473–8.
7. Cooper C, Dunham CM, Rodriguez A. Falls and major injuries are risk factors for thoracolumbar fractures: cognitive impairment and multi injuries impede the detection of back pain and tenderness. J Trauma 1995; 38: 692–6.
8. Riggins RS, Kraus JF. The risk of neurologic damage with fractures of the vertebrae. J Trauma 1977; 17: 126–33.
9. Stover S, Fine P. The epidemiology and economics of spinal cord injury. Paraplegia 1987; 25: 225–8.
10. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery: Part 1. Histologic and histochemical analyses in rats. Spine 1994; 19: 2590–7.
11. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery: Part 2. Histologic and histochemical analyses in humans. Spine 1994; 19: 2598–602.
12. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery: a histologic and enzymatic analysis. Spine 1996; 21: 941–4.
13. Kawaguchi Y, Yabuki S, Styf J, et al. Back muscle injury after posterior lumbar spine surgery: topographic evaluation of intramuscular pressure and blood flow in the porcine back muscle during surgery. Spine 1996; 21: 2683–8.
14. Styf J, Willen J. The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine 1998; 23: 354–8.
15. Jackson RK. The long-term effects of wide laminectomy for lumbar disc excision. J Bone Joint Surg Br 1971; 53: 609–16.
16. Macnab I, Cuthbert H, Godfrey CM. The incidence of denervation of the sacrospinales muscles following spinal surgery. Spine 1977; 2: 294–8.
17. Mayer TG, Vanharanta H, Gatchel RJ, et al. Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine 1989; 14: 33–6.
18. Naylor A. The late results of laminectomy for lumbar disc prolapse: a review after ten to twenty-five years. J Bone Joint Surg Br 1974; 56: 17–29.
19. Rantanen J, Hurme M, Falck B, et al. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine 1993; 18: 568–74.
20. Sihvonen T, Herno A, Paljarvi L, et al. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine 1993; 18: 575–81.
21. Esses SI, Botsford DJ, Wright T, Bednar D, Bailey S (1991) Operative treatment of spinal fractures with the AO internal fixator. Spine (Phila Pa 1976) 16: S146–S150.
22. McLain RF, Sparling E, Benson DR (1993)Early failure of short segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am 75: 162–167.
23. Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, Garfin S (2007) Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976) 32:1503–1507.
24. Li KC, Hsieh CH, Lee CY, et al. Transpedicle body augmenter: a further step in treating burst fractures. ClinOrthopRelat Res 2005; 436: 119–25.
25. Li KC, Li AF, Hsieh CH, et al. Another option to treat Kummell’s disease with cord compression. Eur Spine J 2007; 16: 1479 -87.
26. Raja Rampersaud, Neel Annand, Mark B. Dekutoski. Use of Minimally Invasive Surgical Techniques in the Management of Thoracolumbar Trauma Current Concepts. SPINE 2006; 31, S96–S102.
27. Wild MH, Glees M, Plieschnegger C, Wenda K: Five-year follow-up examination after purely minimally invasive posterior stabilization of thoracolumbar fractures: a comparison of minimally invasive percutaneously and conventionally open treated patients. Arch Orthop Trauma Surg 127: 335–343, 2007.
28. Wang H, Li C, Zhou Y, Zhang Z, Wang J, Chu T: Percutaneous pedicle screw fixation through the pedicle of fractured vertebra in the treatment of type A thoracolumbar fractures using Sextant system: an analysis of 38 cases. Chin J Traumatol 13: 137–145, 2010.
29. Jiang XZ, Tian W, Liu B, Li Q, Zhang GL, Hu L, et al: Comparison of a paraspinal approach with a percutaneous approach in the treatment of thoracolumbar burst fractures with posterior ligamentous complex injury: a prospective randomized controlled trial. J Int Med Res 40:1343–1356, 2012.
30. Andrew J. Grossbach, Taylor J. Abel, Gregory D. Woods, et al. Flexion-distraction injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. Neurosurg Focus 35 (2):E2, 2013.
31. Joseph SA Jr, Stephen M, Meinhard BP: The successful short term treatment of flexion-distraction injuries of the thoracic spine using posterior-only pedicle screw instrumentation. J Spinal Disord Tech 21:192–198, 2008.
32. Panagiotis Korovessis, Eva Mpountogianni, VasilleiosSyrimpeis. Percutaneous pedicle screw fixation plus kyphoplasty for thoracolumbar fractures A2, A3 and B2. Eur Spine J DOI 10.1007/s00586-016, 2016.
33. Chen Z, Zhao J, Xu H, Liu A, Yuan J, Wang C (2008) Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J 17(11):1476–1480.
34. Knox JB, Dai JM 3rd, Orchowski JR (2011) Superior segment facet joint violation and cortical violation after minimally invasive pedicle screw placement. Spine J 11(3):213–217.
35. Zeng ZL, Jia L, Xu W, Yu Y, Hu X, Jia YW, Wang JJ et al (2015) Analysis of risk factors for adjacent superior vertebral pedicle induced facet joint violation during the minimally invasive surgery transforaminal lumbar interbody fusion: a retrospective study. Eur J Med Res 20:80.
36. Rahamimov N, Mulla H, Shani A, Freiman S (2011) Percutaneous augmented instrumentation of unstable thoracolumbar burst fractures. Eur Spine J. doi: 10. 1007/s00586-011-2106-x.
37. Kim DH, Jahng TA, Balabhadra RS, Potulski M, Beisse R: Thoracoscopictransdiaphragmatic approach to thoracolumbar junction fractures. Spine J 4:317–328, 2004.
38. Isaacs RE, Hyde J, Goodrich JA, Rodgers WB, Phillips FM: A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine (Phila Pa 1976) 35 (26 Suppl):S322–S330, 2010.
39. Rodgers WB, Gerber EJ, Patterson J: Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine (Phila Pa 1976) 36:26– 32, 2011.
40. Smith WD, Dakwar E, Le TV, Christian G, Serrano S, Uribe. Minimally invasive surgery for traumatic spinal pathologies: a mini-open, lateral approach in the thoracic and lumbar spine. Spine (Phila Pa 1976) 35 (26 Suppl):S338–S346, 2010.
| How to Cite this Article: Kulkarni A, Ruparel S. Minimally Invasive Spine Surgery Options in Management of Thoracolumbar Fractures- Indications and Surgical Techniques. International Journal of Spine Sep-Dec 2016;1(2):33-38. |