Minimally Invasive Spine Surgery Options in Management of Thoracolumbar Fractures- Indications and Surgical Techniques
Volume 1 | Issue 2 | Sep – Dec 2016 | Page 22-26 | Arvind Kulkarni, Sameer Ruparel
Authors : Arvind Kulkarni [1], Sameer Ruparel [1]
[1] Oyster and pearl hospital, Pune
[2] Jehangir Hospital, Pune
[3] SRM Medical College, SRM University, Kattankulathur, Tamil Nadu 603203
Address of Correspondence
Dr. Rajesh Parasnis
Department of Spine Surgery, Oyster and pearl hospital, India.
Email : rajeshparasnis@rediffmail.com
Abstract
Study Design: Literature review and expert opinion
Objective: Thoracolumbar fractures account for 90% of spine fractures. The conventional surgical treatment consists of open exposure with spinal instrumentation and fusion. With the advent of minimally invasive techniques and their approach related advantages combined with their successful use in degenerative disorders, they are being increasingly used in treatment of thoracolumbar injuries. The objective of this review article is to discuss indications and surgical techniques for the same.
Materials and Methods: A review of current English literature complemented with experience of the senior author was amalgamated.
Results: Current indications and surgical techniques of minimally invasive surgery along with the experience of the author are summarized.
Conclusion: The basic biomechanical principles of treatment of thoracolumbar fractures remain the same, irrespective of the approach. The scope of MIS for treating these injuries is increasing to encompass more complicated fracture patterns.
Key words: spine trauma, thoracolumbar, minimally invasive, instrumentation.
Introduction
Thoracolumbar fractures account for approximately 90% of all spine fractures [1]. Most of these are concentrated between D11 and L2 due to its transition from the rigid, stable kyphotic thoracic spine to mobile, lordotic lumbar spine and thus susceptible to injury. These injuries can result in potentially devastating sequelae including paralysis, pain, deformity, and loss of function [2–5]. In addition to the physical consequences, the long-term effects of spinal injuries may also have a significant psychologic, economic, and social impact [6–9]. The treatment goals for patients with thoracolumbar injuries are to maintain or restore spinal alignment and stability, preserve neurologic function and mobilize the patient as soon as possible. The conventional surgical treatment consists of open exposure with spinal instrumentation and fusion. With the advent of minimally invasive spine surgical techniques and successful utilization for lumbar degenerative disorders, these are increasingly used for the treatment of thoracolumbar fractures. Standard midline posterior spinal approaches have shown to cause significant muscle morbidity resulting from iatrogenic muscle denervation (particularly with exposure lateral to the facet), increased intramuscular pressures, ischemia and revascularization injury [10–14]. All these effects can lead to paraspinal muscular atrophy, scarring, and decreased extensor strength and endurance [15–20]. This approach related morbidity has prompted many spine surgeons to assess the feasibility of minimally invasive spine surgery for the treatment of thoracolumbar fractures. The objective of this review article is to discuss indications and surgical techniques for the same.
Indications and Surgical Technique:
Treatment of thoracolumbar fractures is controversial due to the lack of a classification system which incorporates the mechanism of injury and morphology of the fracture, has good inter observer reliability, neurological status of the patient and the condition of soft tissues. Due to this, it is often difficult to form a definite treatment algorithm for these fractures. However, principles of stabilization and fusion still remain the same irrespective of it being a conventional open or minimally invasive surgery. We used the ASIA scoring system to grade the neurological status of the patient. The AO classification system is used to describe the morphology of the fracture and treatment decision regarding surgery was based the Thoracolumbar Injury Classification and Severity [TLICS] Scale. Patients with progressive neurological deterioration and unstable fractures are frequently operated upon. The use of minimally invasive surgery seems to be a blessing in poly trauma patients requiring stabilization in view of Damage Control Orthopaedics [DCO].
Patients brought to casualty with thoracolumbar fractures are managed according to ATLS protocols. After stabilization, they are thoroughly evaluated and investigated. Classification of fracture and grading of neurological deficit is done as per above mentioned systems. Decision regarding surgery varies from patient to patient, generally patients with TLICS >= 4 are operated. Whether to apply minimally invasive surgical [MIS] techniques to treat these is dependent on numerous factors. MIS techniques are skilful and evidently have a steep learning curve. The surgeon must be thoroughly acquainted with the anatomy of the vertebral structures and MIS equipments. Hospital dependent factors include the availability of microscopes for adequate visualization, trained staff, MIS instrumentation and fluoroscopy. Navigation and use of intraoperative neurophysiological monitoring are additional factors which improve safety of the patient. The most important patient dependent factor is the cost. The benefits of reduced blood loss, infection rates, better tolerance to postoperative pain and faster recovery must be balanced with the cost involved in MIS instrumentation and implants.
Goals of surgery with thoracolumbar fractures include adequate biomechanical stabilization of the fractured segment, decompression of the neural structures and fusion of instrumented vertebrae. These are achieved with conventional open surgeries using anterior/ posterior approaches. Above can be achieved with minimally invasive surgical techniques as follows:
1. Percutaneous pedicle screw fixation- Percutaneous pedicle screw fixation restores the posterior tension band and indirectly augments the anterior column. These can be used when anterior fixation is not feasible and can augment anterior fixation. It is an excellent fixation technique in unstable polytrauma patients for initial stabilization. Typical indications of using these alone include fractures in which anterior column restoration is not required involving posterior elements e.g., Chance fracture i.e. flexion-distraction injuries of the spine.
2. Anterior minimal access decompression and stabilization: Anterior minimally invasive decompression and stabilization can be used independently or augmented with posterior percutaneous pedicle screw fixation and is typically employed in burst fractures wherein reconstruction of anterior column seems to be necessary. Decompression, stabilization and fusion can all be achieved with this approach.
3. Vertebroplasty/Kyphoplasty: This can be combined with percutaneous pedicle screw fixation in cases of pincer, wedge or incomplete burst fractures in middle aged adults, though traditionally vertebropalsty is used for osteoporotic fractures. After indirect reduction with patient positioning, although the vertebral walls give the radiological impression of a good reduction with the pedicle screw construct, the middle part of the endplate cannot be reduced [21]. The adjacent nucleus pulposus may later herniate through the fractured endplate resulting in anterior vertebral column insufficiency, progressive collapse and finally failure [22]. Thus, augmentation with vertebroplasty/ kyphoplasty seems to have a beneficial effect to the discs adjacent to an A3/AO-type fracture, managed with pedicle screw fixation plus endplate restoration, since no significant degeneration occurs 12–18 months post-injury [23].
Often, obtaining adequate anterior column stabilization and fusion with percutaneous pedicle screws and vertebraplasty/kyphoplasty is not feasibile. In these cases anterior approach is mandatory, though in incomplete/complete burst fractures manual reduction and transpedicular body augmentation with titanium spacers combining short segment fixation has been reported to be successful[24,25].
The current uses of MIS techniques and DL injuries where application of MIS can be considered and applied can be summarized as follows: [Table 1 and 2 respectively] by Rampersaud et al [26]:
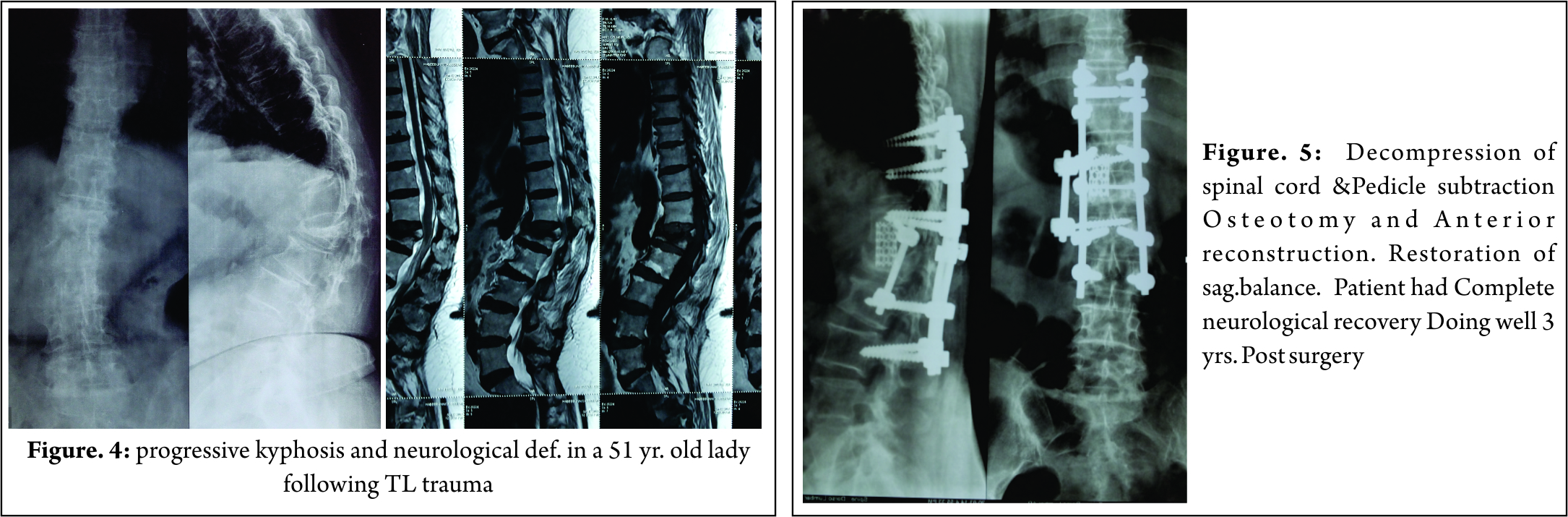
Case Illustrations:
1. A 68 year old lady sustained L1 compression fracture without neurological deficit due to fall [Fig 1]. Patient was treated conservatively for 4 months elsewhere. Patient had persistent pain even after 4 months when repeat x-rays and MRI [Fig 2] showed further collapse of the fractures vertebra and was advised surgery. Patient underwent fixation with percutaneous pedicle screw fixation and vertebroplasty of fractured vertebra [Fig 3].
2. An 89 year old gentleman sustained an L3 vertebral fracture which was treated with vertebroplasty [Fig 4]. Patient complained of pain which was persistent for 4 months post vertebroplasty. Flexion extension x-rays [Fig 5] showed pseudoarthrosis of vertebral fracture, which was then treated with percutaneous cement augmented pedicle screws and vertebroplasty [Fig 6]. Presently, patient is symptomatically better.
3. A 52 year old gentleman suffered chance fracture D3-4 [Fig 7] without neurological deficit which was treated conservatively. 8 months following treatment patient developed myelopathic symptoms with repeat MRI [Fig 8] showing aggravation of radiographic features. Patient was operated with percutaneous pedicle screw fixation D2—5 [Fig 9].
Open Vs MIS in treatment of thoracolumbar fractures:
With increasing use of percutaneous pedicle screw fixation in the treatment of thoracolumbar fractures, studies have been conducted comparing clinical and radiological outcomes with conventional open pedicle screw fixation.
Wild et al in a study of 21 patients of AO Type 3 thoracolumbar compression injuries and concluded that percutaneous pedicle screw instrumentation [PPSI] was associated with significantly less blood loss with no difference in clinical and radiological outcomes 5 years after implant removal. The authors however observed increased operative time with PPSI [27]. Wang et al [28] in their study of 38 patients with similar injuries found significant decreases in operative time also along with other clinical and radiological parameters. While these previous studies retrospectively analysed 2 patient cohorts, Jiang et al. [29] recently published the only prospective randomized control trial comparing PPSI to an open paraspinal approach for thoracolumbar burst fractures in patients without neurological deficits. The authors demonstrated significant decreases in blood loss associated with PPSI compared to the paraspinal approach (79 ml vs 145 ml, respectively), a shorter hospital stay (9.7 vs 10.8 days, respectively) and less pain postoperatively. After more than 3 years of follow-up of 61 patients, there were no differences in Oswestry Disability Index score or VAS score. The paraspinal muscle group was able to achieve and maintain sagittal correction better than those obtained by the PPSI group. The authors concluded that PPSI offers improvements over the paraspinal approach.
Thus, above studies suggest the use of percutaneous pedicle screw instrumentation does have advantages over the conventional open approach whenever feasible.
Another fracture morphology that can be efficiently treated with MIS approaches is patients having flexion- distraction injuries. On comparison of radiological variables with MIS and open approaches, Grossbachet al[30]found though a slight increase in kyphosis [though not statistically significant] in MIS group post operatively. Joseph et al in their study of 15 cases with flexion distraction injuries [31], found that the average kyphosis improved from 19.6° preoperatively to 5.73° postoperatively, a statistically significant difference, and that the degree of kyphosis had increased to 7.87° at last follow-up, an increase that was not statistically significant. The average time to last follow-up was 16.1 months. The authors suggest that thoracic flexion-distraction injury may be amenable to this single surgical approach in most cases.
Many authors have raised concerns about the rates of screw malposition, adjacent facet violation and degeneration with PPSI. Panagiotis Korovessis et al, [32] in their retrospective study of 36 patients, found that 10% screws were malpositioned on axial CT images, four percent with each with grade II and grade III malpositions. Patients with grade III malposition reported lower extremity discomfort without neurological deficit. Intraarticular adjacent segment facet violation by the pedicle screws was disclosed in axial CT images in eight (5.5 %) facet joints. Adjacent joint degeneration at the violated by screw facet was shown in 2 (5.5 %) patients, respectively, 1 year post-operation. Spontaneous inter-facet fusion within the instrumentation area at the 1 year f/up occurred in 10/36 (28 %) patients. On comparison of these statistics with conventional open approach, Chen et al [33] reported 24–100 % facet joint violation rates in open , while other studies reported 11–50 % violation rates for percutaneous procedures [34,35]. However, Panagiotis Korovessis et al, [32] reported much lower facet joint violation rates [5.5%].
PPSI along with vertebroplasty/kyphoplasty for the reconstruction of anterior column has shown good clinical and radiological outcomes. With 18 patients suffering from lumbar compression and burst fractures, Korovessis et al [32] found the mean blood loss and operative times to be 75 ml and 45 minutes respectively. Segmental kyphosis decreased from 16 to 2 degrees with no neurological complications. Though, Rahamimov et at [36] in a similar study found of 52 patients, reported 3 cases of PMMA emboli, and in half of the patients there was a cement leak into adjacent soft tissue either through the fracture or through segmental veins but no cases of extravasation into the spinal canal suggesting potential complications of this technique.
For thoracolumbar injuries with requiring more extensive anterior reconstruction and decompression, Kim et al [37] reported 85% fusion rates for stand alone procedures and 90% for combined procedures. They performed thoracoscopic decompression, reconstruction and instrumentation in 212 patients with AO type A, B and C fractures. However, 64% underwent standard open posterior stabilization. Three cases required conversion to open procedure. 90% patients maintained sagittal alignment at 1 year follow up.
Use of the transpsoas or lateral approach to the lumbar and thoracolumbar spine has been increasing over the last decade in the treatment of degenerative conditions [38, 39]. Smith et al. [40]used this approach in the treatment of 52 patients with AO Type B and C fractures. Expandable titanium cages were used for anterior column support supplemented with anterolateral fixation or pedicle screws or combination of thereof. Mean operative time and blood loss were 127 minutes and 300 ml respectively with complication rates reported to be 15%.
Thus, majority of thoracolumbar fractures are amenable to minimally invasive techniques and these are increasing used successfully for their treatment as evident in above mentioned studies.
References
1. DeWald RL. Burst fractures of the thoracic and lumbar spine. ClinOrthopRelat Res.1984; (189): 150–161.
2. Gertzbein SD. Scoliosis Research Society: Multi center spine fracture study. Spine 1992; 17: 528–40.
3. Levine A, McAfee P, Anderson P. Evaluation and emergent treatment of patients with thoracolumbar trauma. Instr Course Lect 1995; 44: 33–45.
4. McCormack B, MacMillan M, Fessler R. Management of thoracic, lumbar and sacral injuries. In: Tindall G, Cooper P, Barrow D, Eds. The Practice of Neurosurgery. Baltimore: Williams & Wilkins, 1996.
5. Meldon S, Moettus L. Thoracolumbar spine fractures: clinical presentation and the effect of altered sensorium and major injury. J Trauma 1995; 39: 1110–4.
6. Bosch A, Stauffer E, Nichel V. Incomplete traumatic quadriplegia: a ten year review. JAMA 1971; 216: 473–8.
7. Cooper C, Dunham CM, Rodriguez A. Falls and major injuries are risk factors for thoracolumbar fractures: cognitive impairment and multi injuries impede the detection of back pain and tenderness. J Trauma 1995; 38: 692–6.
8. Riggins RS, Kraus JF. The risk of neurologic damage with fractures of the vertebrae. J Trauma 1977; 17: 126–33.
9. Stover S, Fine P. The epidemiology and economics of spinal cord injury. Paraplegia 1987; 25: 225–8.
10. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery: Part 1. Histologic and histochemical analyses in rats. Spine 1994; 19: 2590–7.
11. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery: Part 2. Histologic and histochemical analyses in humans. Spine 1994; 19: 2598–602.
12. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posterior lumbar spine surgery: a histologic and enzymatic analysis. Spine 1996; 21: 941–4.
13. Kawaguchi Y, Yabuki S, Styf J, et al. Back muscle injury after posterior lumbar spine surgery: topographic evaluation of intramuscular pressure and blood flow in the porcine back muscle during surgery. Spine 1996; 21: 2683–8.
14. Styf J, Willen J. The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine 1998; 23: 354–8.
15. Jackson RK. The long-term effects of wide laminectomy for lumbar disc excision. J Bone Joint Surg Br 1971; 53: 609–16.
16. Macnab I, Cuthbert H, Godfrey CM. The incidence of denervation of the sacrospinales muscles following spinal surgery. Spine 1977; 2: 294–8.
17. Mayer TG, Vanharanta H, Gatchel RJ, et al. Comparison of CT scan muscle measurements and isokinetic trunk strength in postoperative patients. Spine 1989; 14: 33–6.
18. Naylor A. The late results of laminectomy for lumbar disc prolapse: a review after ten to twenty-five years. J Bone Joint Surg Br 1974; 56: 17–29.
19. Rantanen J, Hurme M, Falck B, et al. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine 1993; 18: 568–74.
20. Sihvonen T, Herno A, Paljarvi L, et al. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine 1993; 18: 575–81.
21. Esses SI, Botsford DJ, Wright T, Bednar D, Bailey S (1991) Operative treatment of spinal fractures with the AO internal fixator. Spine (Phila Pa 1976) 16: S146–S150.
22. McLain RF, Sparling E, Benson DR (1993)Early failure of short segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am 75: 162–167.
23. Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, Garfin S (2007) Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976) 32:1503–1507.
24. Li KC, Hsieh CH, Lee CY, et al. Transpedicle body augmenter: a further step in treating burst fractures. ClinOrthopRelat Res 2005; 436: 119–25.
25. Li KC, Li AF, Hsieh CH, et al. Another option to treat Kummell’s disease with cord compression. Eur Spine J 2007; 16: 1479 -87.
26. Raja Rampersaud, Neel Annand, Mark B. Dekutoski. Use of Minimally Invasive Surgical Techniques in the Management of Thoracolumbar Trauma Current Concepts. SPINE 2006; 31, S96–S102.
27. Wild MH, Glees M, Plieschnegger C, Wenda K: Five-year follow-up examination after purely minimally invasive posterior stabilization of thoracolumbar fractures: a comparison of minimally invasive percutaneously and conventionally open treated patients. Arch Orthop Trauma Surg 127: 335–343, 2007.
28. Wang H, Li C, Zhou Y, Zhang Z, Wang J, Chu T: Percutaneous pedicle screw fixation through the pedicle of fractured vertebra in the treatment of type A thoracolumbar fractures using Sextant system: an analysis of 38 cases. Chin J Traumatol 13: 137–145, 2010.
29. Jiang XZ, Tian W, Liu B, Li Q, Zhang GL, Hu L, et al: Comparison of a paraspinal approach with a percutaneous approach in the treatment of thoracolumbar burst fractures with posterior ligamentous complex injury: a prospective randomized controlled trial. J Int Med Res 40:1343–1356, 2012.
30. Andrew J. Grossbach, Taylor J. Abel, Gregory D. Woods, et al. Flexion-distraction injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. Neurosurg Focus 35 (2):E2, 2013.
31. Joseph SA Jr, Stephen M, Meinhard BP: The successful short term treatment of flexion-distraction injuries of the thoracic spine using posterior-only pedicle screw instrumentation. J Spinal Disord Tech 21:192–198, 2008.
32. Panagiotis Korovessis, Eva Mpountogianni, VasilleiosSyrimpeis. Percutaneous pedicle screw fixation plus kyphoplasty for thoracolumbar fractures A2, A3 and B2. Eur Spine J DOI 10.1007/s00586-016, 2016.
33. Chen Z, Zhao J, Xu H, Liu A, Yuan J, Wang C (2008) Technical factors related to the incidence of adjacent superior segment facet joint violation after transpedicular instrumentation in the lumbar spine. Eur Spine J 17(11):1476–1480.
34. Knox JB, Dai JM 3rd, Orchowski JR (2011) Superior segment facet joint violation and cortical violation after minimally invasive pedicle screw placement. Spine J 11(3):213–217.
35. Zeng ZL, Jia L, Xu W, Yu Y, Hu X, Jia YW, Wang JJ et al (2015) Analysis of risk factors for adjacent superior vertebral pedicle induced facet joint violation during the minimally invasive surgery transforaminal lumbar interbody fusion: a retrospective study. Eur J Med Res 20:80.
36. Rahamimov N, Mulla H, Shani A, Freiman S (2011) Percutaneous augmented instrumentation of unstable thoracolumbar burst fractures. Eur Spine J. doi: 10. 1007/s00586-011-2106-x.
37. Kim DH, Jahng TA, Balabhadra RS, Potulski M, Beisse R: Thoracoscopictransdiaphragmatic approach to thoracolumbar junction fractures. Spine J 4:317–328, 2004.
38. Isaacs RE, Hyde J, Goodrich JA, Rodgers WB, Phillips FM: A prospective, nonrandomized, multicenter evaluation of extreme lateral interbody fusion for the treatment of adult degenerative scoliosis: perioperative outcomes and complications. Spine (Phila Pa 1976) 35 (26 Suppl):S322–S330, 2010.
39. Rodgers WB, Gerber EJ, Patterson J: Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine (Phila Pa 1976) 36:26– 32, 2011.
40. Smith WD, Dakwar E, Le TV, Christian G, Serrano S, Uribe. Minimally invasive surgery for traumatic spinal pathologies: a mini-open, lateral approach in the thoracic and lumbar spine. Spine (Phila Pa 1976) 35 (26 Suppl):S338–S346, 2010.
| How to Cite this Article: Kulkarni A, Ruparel S. Minimally Invasive Spine Surgery Options in Management of Thoracolumbar Fractures- Indications and Surgical Techniques. International Journal of Spine Sep-Dec 2016;1(2):33-38. |